Introduction:
3D printing represents a transformative leap in manufacturing, allowing for the fabrication of intricate shapes and geometries directly from digital models. Its precision, accuracy, and versatility across a wide range of printable materials have revolutionized various industries, offering cost-effective and efficient solutions for producing both prototypes and finished products.
The advent of patient-specific medical equipment, tailored to individual anatomies through 3D printing, has significantly enhanced clinical care in fields such as medicine and dentistry. Traditional subtractive manufacturing processes are unable to match the customization and versatility offered by additive manufacturing methods like 3D printing.
Furthermore, the emergence of 3D bioprinting holds the potential to revolutionise transplantation and tissue replacement by enabling the replication of biological tissues and organs. Moreover, the digitization of workflows and the application of stereolithography techniques have brought about significant advancements in dental practices.
Despite the prevalence of light-cured resin in dental applications, other 3D printing methods such as FDM and SLS offer alternative solutions. Processes involving resin curing have played a pivotal role in making dental 3D printing.
This paper aims to trace the evolution of Stereolithography (SLA) and Digital Light Processing (DLP) technologies inherent in dental 3D printing, emphasising their impact on dentistry and related medical fields. By examining the 3D printing mechanism and the array of printable materials in dentistry that are available, this study elucidates the utilisation of this technology across various dental specialties.
3D Printing Technologies:
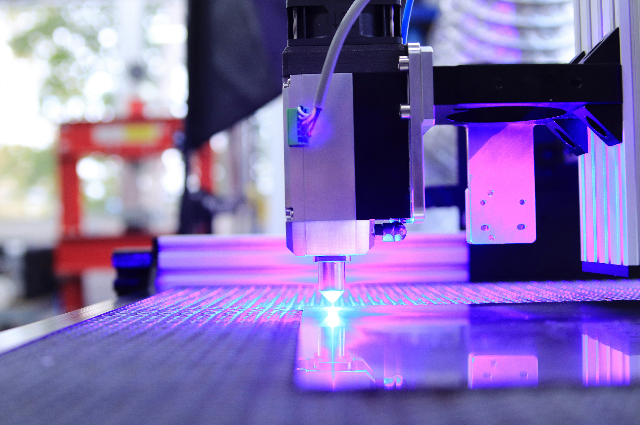
- Stereolithography (SLA): Renowned for its speed, precision, and versatility, SLA employs photochemical techniques that result in highly accurate designs because of layer by layer liquid resins curing. Despite its extended beam-curing process, SLA consistently delivers smooth and precise products, making it a staple in dentistry for crafting patient-specific crowns, dentures, surgical guides, and diagnostic models. (Figure 01)
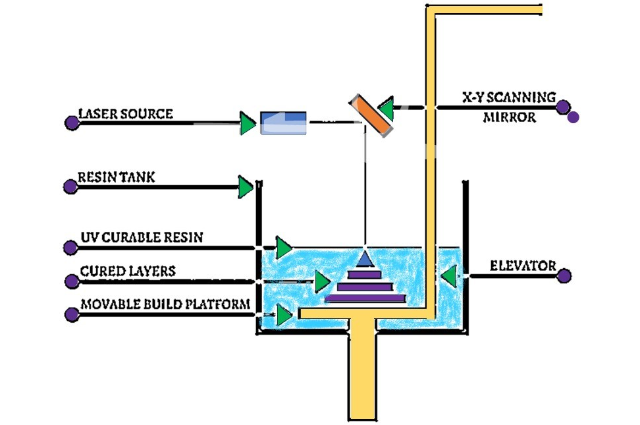
- Digital Light Processing (DLP): Addressing the issue of prolonged fabrication times, DLP utilises photopolymer resins cured layer by layer with a light source, facilitating the creation of intricate designs with precision. DLP outpaces SLA in terms of speed, as entire layers are cured with a single flash. The resolution of DLP prints is determined by the size of voxels, with larger voxels leading to decreased resolution. Widely employed in dentistry, DLP technology aids in the production of crowns, dentures, and prosthetic devices, streamlining clinical procedures and enhancing outcomes of treatment.
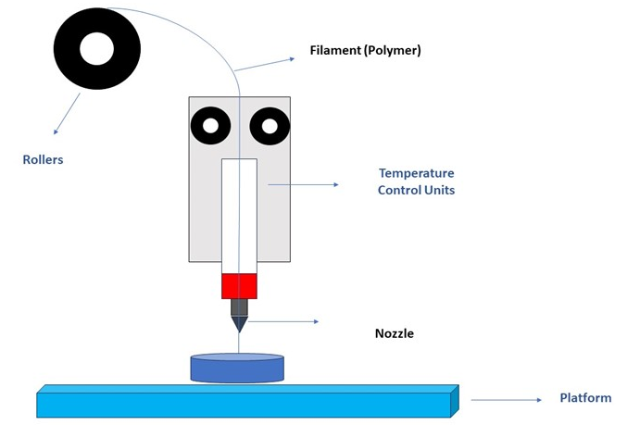
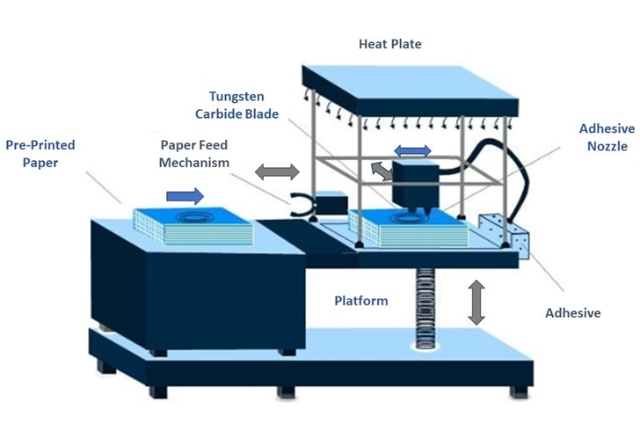
- Fused Deposition Modeling (FDM): A versatile printing method utilised across various healthcare applications, FDM involves the extrusion and deposition of semi-solid thermoplastic filaments layer by layer. While FDM achieves strong layer bonding, its compatibility is limited to thermoplastics. (Figure 02)
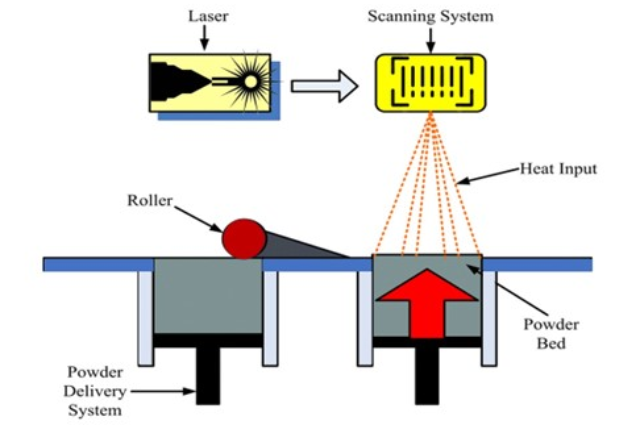
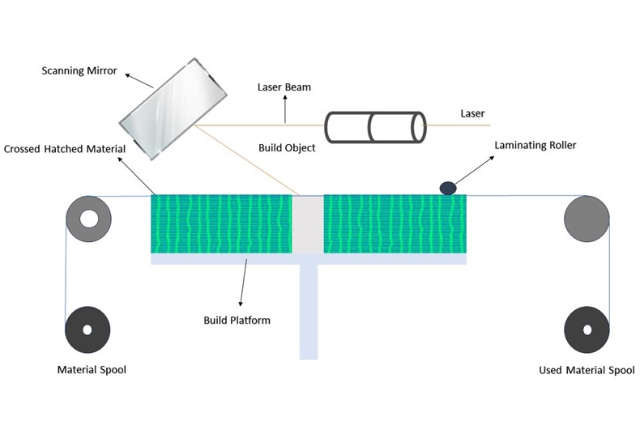
- Selective Laser Sintering (SLS): Offering time-saving benefits, SLS selectively fuses the powdered ceramic, metals, and polymers by employing a high-temperature laser resulting in high-density, dental-grade materials. Although requiring extensive infrastructure, SLS finds application in dentistry for fabricating frameworks for removable partial dentures, minimising errors and providing a safer alternative to traditional casting methods. (Figure 03)
- Photopolymer Jetting Printing (PolyJet 3D printing): Characterised by its ability to print in multiple colours, PolyJet 3D printing is particularly advantageous in esthetic dentistry. Inkjet printheads dispense fusing agent droplets onto a powder bed, followed by curing with infrared lamps. While offering multi-material printing capabilities, PolyJet 3D printing necessitates frequent print head maintenance and exhibits limited mechanical properties for dental applications.
- Powder Binder Jetting: Utilizing biocompatible elastomers and medical-grade silicones, powder binder printing is suitable for maxillofacial prostheses. A silicone polymer-infiltrated water-based binder selectively bonds layers of starch-based powder, yielding patient-specific designs. However, the mechanical properties of powder binder prints are relatively weak, constraining their use in dentistry.
- Laser Bioprinting (LAB): Integrating additive manufacturing with biotechnology, LAB holds promise for dental regenerative therapies. By layering living cells and biomaterials using lasers, LAB facilitates the creation of tissue-engineered constructs for oral mucosal restoration and periodontal regeneration, offering solutions to challenging dental issues and enhancing patient health.
The rapid improvement of dental 3D printing materials is focused on enhancing mechanical properties and biocompatibility, akin to conventional resins. These resins undergo refinement through curing and washing processes, further enhancing their suitability for dental applications.
Dental 3D Printing Applications - Prosthodontics
Crown and Fixed Partial Dentures (FPDs)
Prosthodontics has shown increasing interest in 3D printing technologies, particularly SLA and DIP, for fabricating definitive or provisional crowns and FPDs. Intraoral scanning of prepared implant and teeth scan bodies enables the creation of precise virtual models, which are then used for prosthesis design using CAD software (e.g., 3Shape Dental System 2022, 3Shape A/S, Copenhagen, Denmark). Utilizing 3D printing for prosthesis production offers advantages in terms of cost-effectiveness, speed, and resource efficiency compared to milling methods. Some studies have demonstrated superior edge and internal fit of 3D-printed provisional crowns compared to milled counterparts.
Full and Removable Partial Dentures
The fabrication of dentures can pose challenges in patients with conditions such as severe gag reflex, TMJ disorders, tumour excision, or oral abnormalities, despite advancements in denture materials and techniques. In recent years, the integration of intraoral scanning and 3D printing has streamlined denture manufacturing, minimising traditional laboratory stages, reducing errors, and enhancing flexibility. Traditional methods involving waxing and investing for removable partial denture (RPD) frameworks are time-consuming and prone to technique sensitivity and complications, such as wax and cast deformation leading to misalignment, pressure-induced mucosal ulcers, and ridge resorption. Studies have indicated that RPD frameworks fabricated via selective laser melting (SLM) exhibit superior fit compared to those produced through lost-wax and metal casting methods. Additionally, 3D-printed frameworks have been associated with more homogeneous contact pressure, mitigating resorption of the residual ridge.
Implantology 3D printing technology is utilised in implantology to simplify and optimise surgical procedures, improving predictability and accuracy while enhancing efficiency and reducing the risks involved. Traditional surgical guides, those based on 2D panoramic radiographs, often suffer from inaccuracies due to low resolution and distortion. Advanced digital technology allows for the generation of surgical guides using CAD software based on cone beam computed tomography (CBCT) and intraoral images, which are then manufactured using 3D printing. This approach has been shown to enhance the accuracy of 3D-printed surgical guides compared to traditional methods. Furthermore, 3D-printed surgical guides offer advantages in terms of cost, speed, simplicity, and customization to the patient's anatomy.
Dental/Maxillofacial Surgical Templates and Guides
For 30 years, oral and maxillofacial dentistry has leveraged additive manufacturing for various purposes, including model construction, diagnosis, surgery planning, and the fabrication of surgical templates and guides, as well as bespoke implant production. CT imaging and CAD software analysis of maxillomandibular defects are utilised to generate surgical guides and templates, akin to the process for 3D-printed implant surgical guides. These personalised guides and templates enhance surgical precision, margin control, and bone preservation, thereby reducing errors and improving outcomes.
Custom Implants
Custom dental implants, designed and fabricated using 3D printing technology, offer the advantage of complex geometries. Technologies such as SLS and SLM enable the printing of titanium or implantable polymers, such as polyether ether ketone, allowing for implants with mechanical properties and with adjustable porosity. While pressing and milling methods offer benefits such as predictable use of homogeneous materials, reduced post-processing, 3D printing is often integrated with these techniques to create implants.
Maxillofacial Prostheses
3D printing has the capability to produce intricate geometries makes it invaluable in crafting prostheses for maxillofacial abnormalities. Scanning and 3D printing enable the fabrication of accurate and comfortable prostheses tailored to match the defect, with the additional benefit of reduced production time and improved reproducibility for various prostheses.
Orthodontics
Orthodontic aligners for malocclusion are predominantly manufactured via 3D printing, offering advantages in terms of clarity, removability, dental hygiene, and aesthetics compared to traditional braces. While previous methods relied on SLA or FDM printing of models followed by thermoforming of aligners from thermoplastic materials, direct 3D printing of aligners is becoming increasingly prevalent due to improved fit, function, and reproducibility without altering material properties. Based on studies assessing accuracy, load resistance, and deformation, direct 3D-printed aligners have been found to be more stable than thermoformed ones. Gnathology utilises 3D printing to address temporomandibular disorders (TMDs), with digital planning of therapeutic interventions based on kinematic tracing records and the fabrication of tailored intraoral appliances using 3D printing technology, thereby enhancing precision.
Endodontics
Endodontics, like other branches of dentistry, benefits from 3D printing technology, with applications ranging from access cavity preparation to teaching and training. Studies have demonstrated the accuracy of 3D-printed access guides for guided cavity preparation, with minimal deviations from planned access points. Guided apicoectomy, a procedure requiring targeted osteotomy and root excision, also benefits from 3D-printed surgical guides, resulting in improved precision compared to freehand methods.
Periodontics
Regenerative Hard and Soft Tissue Scaffolds
Periodontics utilises 3D printing for the regeneration of both soft and hard tissues, as well as surgeries like gingivectomy which are by guided method. Research in this area has focused on the development of 3D-printed scaffolds for regeneration of bone and periodontal tissues, offering customised additive biomanufacturing that enhances bone contact and improves healing and aesthetics compared to traditional scaffolds. Additionally, 3D printing enables the fabrication of soft tissue grafts for keratinized tissue augmentation, addressing larger and more intricate lesions without constraints associated with donor sites.
Gingivectomy Surgery Guides
Surgical guides for gingivectomy and smile design are commonly 3D printed in periodontics, allowing for the creation of patient-specific aesthetic gingivectomy surgical guides using intraoral scanning and CAD software. These guides enhance surgical precision, accuracy, and customization, thereby improving aesthetics.
Future Directions:
The growth of 3D printing in dentistry is attributed to its precision, efficiency, and accessibility. As materials and printing technology are advancing, we anticipate the emergence of personalised prostheses and biomaterials. Dental professionals are actively exploring the integration of 4D printing, enabling printed materials to change shape in response to environmental stimuli. This innovation holds the potential for biomaterials capable of adapting to complex tissue abnormalities and temperature-responsive repairs. Fourth-dimensional printing may facilitate the development of endodontic devices with shape memory to prevent separation and dental implants with hardness conducive to nerve protection. Additionally, computed axial lithography emerges as a promising approach for expedited production using low-viscosity materials. The ongoing advancement of technology and materials will continue to shape the impact of 3D printing on dentistry.
Conclusion:
This essay provides an overview of the history, methods, advantages, and limitations of dental 3D printing. Across interdisciplinary dentistry, the applications of 3D printing technology and materials are expanding. While current accuracy and quality are subject to constraints, ongoing research efforts are poised to enhance 3D printing in dentistry, thereby improving patient care, education, and research endeavours.
