
Photo by Leyre on Unsplash
Highlights of Xerostomia
Xerostomia, also known as dry mouth, is a common condition characterized by a lack of saliva production. Some of the highlights of xerostomia include:
- Causes: Xerostomia can be caused by medications, radiation therapy, Sjogren's syndrome, or other underlying medical conditions.
- Symptoms: The most common symptom of xerostomia is a persistent feeling of dryness in the mouth. Other symptoms include difficulty speaking and swallowing, increased thirst, and a change in taste perception.
- Complications: Xerostomia can increase the risk of oral health problems, such as tooth decay, gum disease, and thrush (a fungal infection of the mouth).
- Treatment: Treatment for xerostomia may include lifestyle changes, such as drinking more water, avoiding alcohol and tobacco, and using saliva substitutes. In severe cases, medications may be prescribed to increase saliva production.
- Prevention: To prevent xerostomia, it is important to maintain good oral hygiene and to avoid medications that can cause dry mouth. Drinking plenty of water and avoiding caffeine and alcohol can also help.
Introduction:
Xerostomia, also known as dry mouth, is a condition characterized by a reduction or lack of salivary secretion, resulting in a subjective feeling of dryness in the mouth. It was first described by Bartley and is not considered a specific disease, but rather a symptom associated with various underlying causes such as autoimmune diseases, medication use, and radiation therapy for cancer treatment. Xerostomia is common among elderly individuals and can cause difficulty in swallowing, and speaking, burning sensations, altered taste, bad breath, and oral soreness.
This condition can also lead to an increased risk of dental cavities and periodontal diseases, as well as oral infections such as candidiasis. Xerostomia can significantly impact a patient's emotional and social well-being and overall quality of life.
Diagnosis of xerostomia is based on a patient's history and physical examination, and treatment aims to alleviate symptoms, although a complete cure may not always be possible. It is important for healthcare professionals to recognize and take seriously the prevalence of xerostomia in the general population, as patients may feel their symptoms are not being acknowledged or addressed.
It is crucial for healthcare professionals to be aware of the prevalence of xerostomia among the general population. Nedefors pointed out that if objective tests do not match the patient's complaints, they may feel that their symptoms are not being taken seriously and may even be dismissed by medical and dental professionals.1
- Definition:
Xerostomia, also known as dry mouth, is a condition characterized by a lack of saliva in the mouth. It is not a disease, but rather a symptom that can be caused by various medical conditions, radiation therapy to the head and neck, or certain medications. It may or may not be linked to reduced function of the salivary glands.
- Epidemiology:
The impact of xerostomia on oral health has been studied for many years, but the true prevalence of this disorder in the general population is still debated. The rate of xerostomia can vary in different countries and ethnic groups, and it is estimated to be as high as 50% in certain subpopulations.2
In general, the rate of xerostomia increases as people age, with an estimated 30% of individuals aged 65 and older experiencing it. The incidence of xerostomia is also very high among patients with Sjogren's Syndrome (SS), a condition in which the immune system attacks the body's moisture-producing glands, which affects between 1-4% of older adults.3
The prevalence of xerostomia is slightly more common in female patients than in male patients, which may be attributed to the smaller size of their salivary glands and a lower salivary flow reserve. Additionally, older age groups are more likely to experience xerostomia than younger age groups, possibly due to increased use of medications and the presence of other health conditions. Studies on the prevalence of xerostomia in the general population have reported rates ranging from 0.9% to 64.8% and 9.7% according to a study by Pujol et al.4,5
A study by Pinto VL et al found a high prevalence of xerostomia among women with breast cancer, regardless of the chemotherapy regimen used. Factors such as age, tobacco and alcohol use, and the use of medications such as antihypertensives, analgesics, oral antidiabetics, and corticosteroids were not found to influence the prevalence of xerostomia. However, the use of antiemetics was found to contribute to the development of xerostomia in the third and final session of the study.6
- Pathophysiology:
Xerostomia can be caused by two main factors: changes in the structure of the salivary glands or changes in their function. Structural changes can occur due to diseases that destroy the gland tissue, resulting in reduced saliva production, such as infections, autoimmune disorders, and radiation therapy. Functional changes occur when there is a decrease in saliva production with normal gland tissue or changes in the consistency of saliva caused by factors such as medications, dehydration, lack of stimulation, and habits such as smoking. Stimulation of the oral mucosa sends signals to the salivary glands in the brain, activating the release of a chemical called acetylcholine, which increases saliva production and flow. Other factors, such as taste, smell, and anxiety, can also influence salivation.7
Histological Changes
Waterhouse and his team conducted studies on the structure of the human submandibular salivary glands using a method called morphometry.8 Their study revealed that as people age, functional cells within the submandibular salivary glands are replaced by fat and connective tissue. On average, they found that in individuals over 75 years old, 25% fewer functional cells were present compared to those under 14 years old. These findings were later supported by studies of Scott according to a morphometric study, it was determined that the decrease in parenchymal volume in older individuals is caused by a reduction in acinar tissue and an increase in the volume of the ducts in the glands.9 Although these studies show that changes do occur in the structure and function of salivary glands as people age, there is currently no evidence to suggest that dry mouth is caused solely by the aging process. However, the loss of functional cells can reduce an older person's ability to compensate for any additional factors that may further decrease saliva flow. Despite this, dry mouth is a common complaint among older individuals. The factors that contribute to dry mouth and the problems it causes in older people are still not well understood.
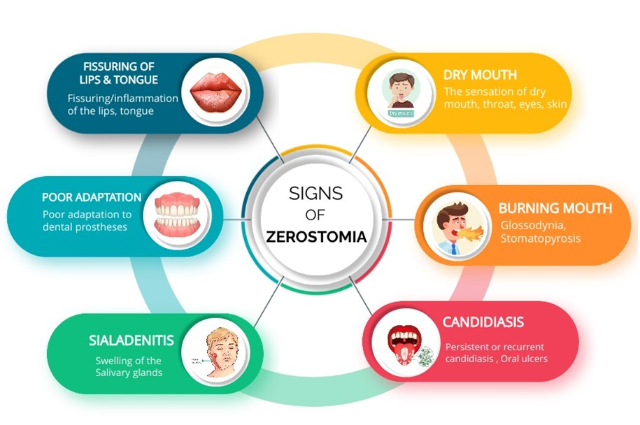
Signs and Symptoms:
Dry mouth can lead to a variety of symptoms, including pain while swallowing (odynophagia), difficulty swallowing (dysphagia), bad breath (halitosis), altered taste (dysgeusia), difficulty speaking (dysarthria), difficulties with speech, and a burning sensation in the mouth. (Figure 1) Physical examination may reveal angular cheilitis, a smooth tongue, cavities, and oral yeast infections. Additionally, dry mouth can lead to long-term complications such as difficulty adapting to dental prosthetics, frequent ulcerations and increased risk of oral infections. It is important to consider the underlying cause of the dry mouth, as it may have additional symptoms.10
Table 1: Sings and Symptoms of Xerostomia (11)
| Sings | Symptoms |
| The sensation of dry mouth, throat, eyes, skin | Dysgeusia (Altered taste), |
| Viscous, Sticky Saliva or thick saliva | Gingivitis |
| Burning mouth (glossodynia, stomatopyrosis) | Altered Sense of smell |
Persistent or recurrent | Difficulty speaking |
| Swelling of the Salivary glands | Chewing and swallowing difficulty |
| Candidiasis | Increase in destructive dental caries/ decay |
| Poor adaptation to dental prostheses | Dental erosions (in the form of |
| Fissuring/inflammation of the lips, tongue | Retrosternal pain due to gastroesophageal reflux |
| Poor nutrition |
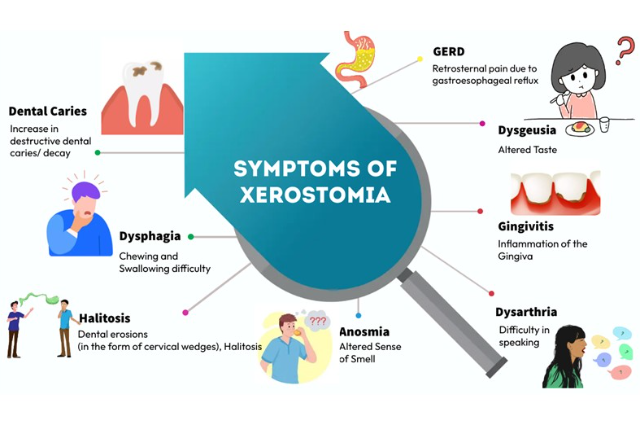
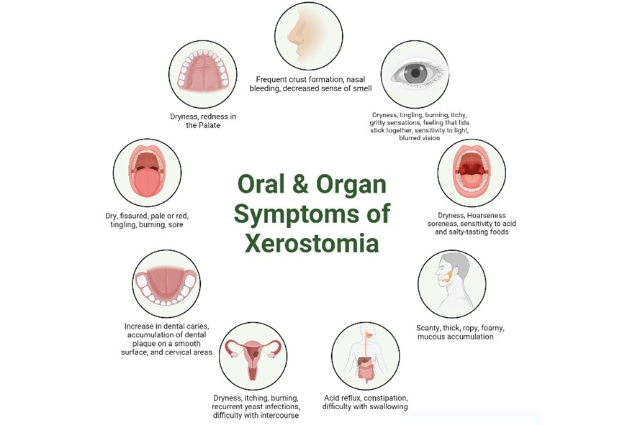
The severity of symptoms increases as the volume of saliva decreases. Other organs such as the nose, eyes, throat, gastrointestinal tract, and vagina can also be affected. (Figure 3A) Symptoms include dryness and itching in the oral cavity and other organs. (Figure 2)
Table 2: Oral and other organ Symptoms of Xerostomia(12)
| Associated Oral Symptoms | Associated General Symptoms |
| ORGANS | ORGANS |
| MOUTH- soreness, sensitivity to acid and salty-tasting foods | NOSE - frequent crust formation, nasal bleeding, decreased sense of smell |
| SALIVA - scanty, thick, ropy, foamy, mucous accumulation | EYES - dryness, tingling, burning, |
| CHEEKS - dry, rough, coated | THROAT - dryness, hoarseness |
| TONGUE - dry, fissured, pale or red, tingling, burning, sore | G.I. TRACT - acid reflux, constipation, difficulty with swallowing |
| PALATE - dryness, redness | VAGINA - dryness, itching, burning, recurrent yeast infections, difficulty with intercourse |
| SALIVARY Glands: swollen, obstructed, non-tender or painful | |
| Teeth: increase in dental caries, accumulation of dental plaque on a smooth surface, and cervical areas | |
| ORAL FUNCTIONS | GENERALIZED SYMPTOMS |
THIRST: frequent sipping of water, especially when eating, need to keep water at the bedside at night | Fatigue, weakness, loss of weight, anxiety, depression, painful joints, multi-drug use symptoms |
TASTE AND SMELL: diminished ability to taste foods, problems with smell | |
MASTICATION: difficulty with the ability to eat dry foods, difficulty with bolus formation, difficulty with the denture, difficulty in swallowing, and needs to sip water while eating | |
SPEECH: difficulty with talking, hoarseness, tongue sticks to the palate |
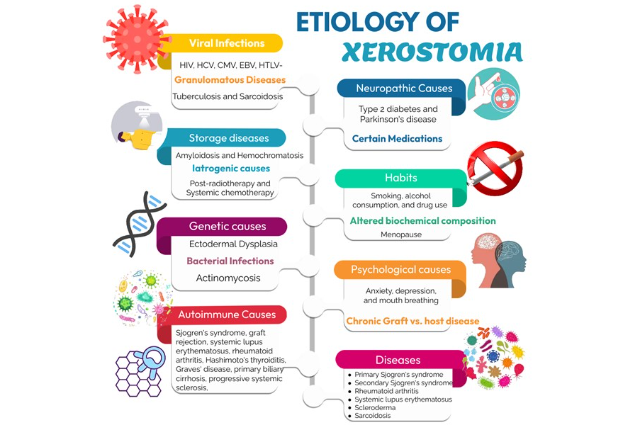
Etiology and Classification:
Xerostomia, or dry mouth, can have various causes (Figure 3B), including the use of certain medications, Sjogren's syndrome, and post-radiotherapy. The causes of xerostomia can be classified into two main categories: glandular structural alteration and functional causes.13
Glandular structural alteration causes include:
Inflammatory and immune-mediated causes such as viral infections (HIV, HCV, CMV, EBV, HTLV-I) and autoimmune diseases (Sjogren's syndrome, graft rejection, systemic lupus erythematosus, rheumatoid arthritis, Hashimoto's thyroiditis, Graves' disease, primary biliary cirrhosis, progressive systemic sclerosis, granulomatosis with polyangiitis, mixed connective tissue disease).
- Granulomatous diseases such as tuberculosis and sarcoidosis.
- Storage diseases like amyloidosis and hemochromatosis.
- Iatrogenic causes such as post-radiotherapy and systemic. chemotherapy.
- Genetic causes like ectodermal dysplasia.
- Bacterial infections like actinomycosis.
Functional causes include:
- Dehydration due to conditions such as chronic kidney disease, type 2 diabetes, and chronic diarrhea.
- Psychological causes like anxiety, depression, and mouth breathing.
- Habits such as smoking, alcohol consumption, and drug use (cocaine, amphetamines).
- Altered biochemical composition of saliva due to menopause.
- Neuropathic causes like type 2 diabetes and Parkinson's disease.
Medications with anticholinergic effects, sympathomimetics, bronchodilators, antiparkinsonian drugs, antidepressants, antipsychotics, decongestants, antihistamines, mydriatics, urinary incontinence drugs, diuretics, antihypertensives, muscle relaxants, opioid pain relievers, non-steroidal anti-inflammatories, proton-pump inhibitors, antiemetics, and antiretrovirals.
In older adults, the occurrence of dry mouth is more common due to a combination of factors including age-related decreased function, illnesses that cause dehydration, the use of multiple medications, a history of smoking, and autoimmune diseases such as Sjogren's syndrome which can lead to parotid carcinoma requiring postoperative radiation therapy.14
When the cause of dry mouth is not known, it is important to consider potential causes such as neurological issues, changes in the composition of saliva, shrinkage of salivary glands and lichen planus.15
Research has shown that individuals with xerostomia have altered levels of certain components in their saliva, such as increased potassium, chloride, calcium, immunoglobulin A, and amylase. In menopausal women, who often experience xerostomia, the levels of estrogen and progesterone are low and there are high levels of calcium and cortisol, which may be linked to hormonal changes in the body. This suggests that changes in hormone levels in the blood may be a contributing factor to xerostomia.
Iatrogenic causes of xerostomia include: 16
- Medications such as radiotherapy to the head and neck, systemic chemotherapy, and bone marrow transplantation.
- Chronic Graft vs. host disease.
Diseases that can affect the salivary glands and cause dry mouth include:
- Primary Sjogren's syndrome
- Secondary Sjogren's syndrome
- Rheumatoid arthritis
- Systemic lupus erythematosus
- Scleroderma
- Diabetes mellitus type 1 or 2
- Sarcoidosis
- HIV disease (AIDS)
- Primary biliary cirrhosis
Other possible causes include:
- Anxiety or depression
- Amyloidosis
- Wegeners granulomatosis
- Primary biliary cirrhosis (PBC)
The Mason and Chisholm Classification for the etiology of Xerostomia categorizes the causes of dry mouth based on four main factors: those that affect the salivary center, the autonomic outflow pathway, salivary gland function, and changes in fluid or electrolyte balance.17
Factors affecting the salivary center:
- Emotions such as fear, excitement, and depression
- Neuroses and endogenous depression
- Organic diseases such as brain tumors
- Certain medications
Factors affecting the autonomic outflow pathway:
- Encephalitis
- Brain tumours
- Accidents
- Neurosurgical operations
- Certain medications
Factors affecting salivary gland function:
- Apiesia (loss of the ability to produce saliva)
- Sjogren's syndrome
- Obstruction
- Infection
- Irradiation
- Excision
- Factors producing changes in fluid or electrolyte balance:
- Dehydration
- Diabetes insipidus
- Cardiac failure
- Uremia
- Edema
Other factors that may contribute to the development of xerostomia include cigarette smoking, changes in taste sensation, frequent snacking, poorly controlled diabetes, chronic graft vs host disease, thyroid disorders, hepatitis C, Milkulicz's disease (a condition characterized by inflammation of glands in the head and neck), surgical removal of salivary glands, dehydration, psychological conditions such as fear, anxiety and depression, mouth breathing, nasal obstruction, damage to head and neck that affects the nerves that control the salivary glands, and candidiasis.18
Method of detection:
In order to evaluate and diagnose xerostomia, a medical professional will examine the oral mucosa and ask questions about any dryness complaints the patient may have. They will also gather information about any systemic or local diseases, past trauma, and medications being taken. Specific questions will be asked to assess symptoms that can indicate hyposalivation, such as difficulty swallowing or a dry mouth when eating. A physical examination will be conducted, which includes examination of the major salivary glands, lymph nodes, and other oral structures such as the soft tissues, periodontium, and dentition. Measurement of salivary output, sialo chemical analyses, blood tests, and imaging techniques such as sialography, scintigraphy, ultrasonography, MRI, CT scan, and salivary biopsy may also be done in order to fully evaluate and diagnose xerostomia.19
Xerostomia is diagnosed through a combination of patient history and physical examination. One key indicator of xerostomia is a salivary flow rate that is less than half of the normal rate. During the patient history examination, questions are typically asked about dry mouth, difficulty swallowing, and perceived decrease in saliva production. In the physical examination, both extraoral and intraoral examination are conducted. The extraoral examination includes examination of the major salivary glands and lymph nodes. Enlarged, bilateral, non-tender major salivary glands may be observed, and the examiner may not be able to express saliva from the submandibular or parotid ducts.16
An intraoral examination is crucial in identifying the specific clinical signs that are indicative of hyposalivation. The examination includes the examination of soft tissues, gums, and hard tissues. Osailan et al have proposed several signs that can help in the diagnosis, such as: 1) the sticking of an intraoral mirror to the cheek or tongue; 2) frothy saliva; 3) lack of saliva pooling in the floor of the mouth; 4) loss of papillae on the tongue; 5) altered or smooth gum architecture; 6) glassy appearance of the oral mucosa, particularly the palate; 7) a lobulated or deeply fissured tongue; 8) more than two teeth with cervical caries; and 9) mucosal debris on the palate (except under dentures).20
Patients with decreased salivary flow, or hyposalivation, may experience swelling of one or both of their salivary glands. This condition is known as sialadenitis. This can be caused by a variety of factors, including infection, radiation therapy, and certain medications. Individuals with Sjogren's syndrome, an autoimmune disorder, may also experience sialadenitis without infection due to dryness in the mouth and eyes. It is important to consult a healthcare professional if you have concerns about enlarged salivary glands.19
After a physical examination, the next step in assessing salivary flow is to measure the actual amount of saliva being produced. There are a variety of methods for measuring salivary flow, most of which are easy to perform and take very little time. The flow rates are typically measured for at least 5 minutes after an overnight fast or 2 hours after a meal. It is important to measure salivary flow at different times of the day and after different stimuli in order to get the most accurate measurement of salivary function.21
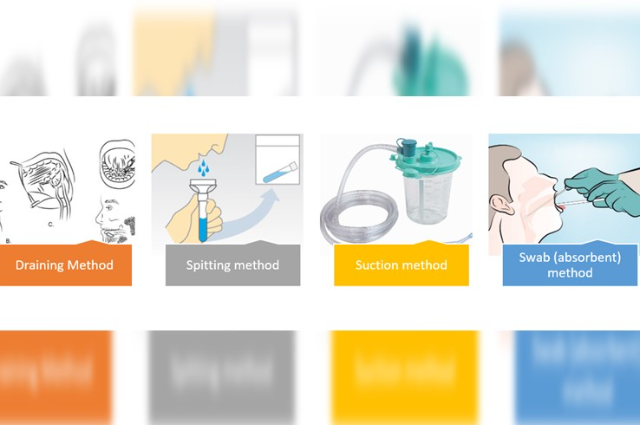
There are four main methods commonly used to collect whole saliva: (Figure 4B)
The draining method: Saliva is collected by allowing it to drip off the lower lip into a pre-weighed or graduated test tube fitted with a funnel. The subject expectorates into the test tube at the end of the collection period.
The spitting method: Saliva is allowed to accumulate on the floor of the mouth, and the subject spits it out into a pre-weighed or graduated test tube every 60 seconds.
The suction method: Saliva is continuously drawn from the floor of the mouth into a test tube using a saliva ejector or an aspirator.
The swab (absorbent) method: Saliva is collected by using a pre-weighed swab, cotton roll, or gauze sponge placed in the mouth at the orifices of the major glands and removed for re-weighing at the end of the collection period.22
There are several techniques available to assess the dryness of the mouth, including sialography, sialochemistry, sialometry, scintigraphy, salivary gland biopsy, ultrasound, magnetic resonance imaging, and computed tomography. These methods are used to evaluate the level of dryness of the mouth and provide a better understanding of the underlying condition.23
Sialography is a diagnostic imaging technique that involves injecting radiopaque material into the salivary ducts retrogradely to visualize the anatomy of the glands. This test is useful in identifying the presence of nodules or sialectasis, but it has some drawbacks such as being an invasive procedure, and some patients may have adverse reactions to the contrast material. A biopsy of the major or minor salivary glands, on the other hand, can detect inflammation, destruction of the glands, and the presence of thick mucus and fibrosis in the salivary ducts.24
Diagnosis of salivary gland disease can also be done using imaging techniques such as computed tomography, magnetic resonance imaging and ultrasound. These tests are complementary to the others and help to evaluate the involvement of salivary glands in patients with xerostomia. (Figure 4A)
Sialometry is a relatively common procedure in clinical practice and includes the measurement of stimulated salivary flow rate (s-SFR), unstimulated salivary flow rate (u-SFR), palatal secretion (PAL), and parotid secretion (PAR). These methods are simple and help to evaluate salivary gland function by measuring the amount of saliva produced per unit of time. Very low unstimulated and stimulated salivary flow rates, or hyposalivation, are defined as <0.1 and <0.7 ml/min. respectively.25 The amount of saliva produced by the submandibular and sublingual glands at rest typically ranges from 0.25 to 0.35 mL/min.26
When stimulated, the parotid glands are responsible for producing 50% of the total volume of saliva.27 The amount of saliva produced by an individual at a given time is measured by measuring the stimulated and unstimulated salivary flow. Typically, the stimulated salivary flow is measured for 5 minutes and the unstimulated salivary flow is measured for 15 minutes.28
The benefits of measuring salivary flow in this manner include ease of implementation, low cost, and accessibility to a large portion of the population at risk.29
A definitive diagnosis of glandular pathology can be made through a salivary gland biopsy. A biopsy of the minor salivary glands, located in the lips, is a more common and easily performed procedure than a biopsy of the major salivary glands.30
Fine-needle aspiration biopsy of the major salivary glands, which are enlarged, followed by immunocytochemical analysis, is an effective method for distinguishing benign polyclonal lymphocytic infiltration from malignant monoclonal infiltration, as in the case of lymphoma.19
Table 3: Summary for Method of Detection of Xerostomia:
| Sr. No | Method of detection of xerostomia |
| 1. | History: A patient's medical history including any medications |
| 2. | Salivary Flow Rate test: done by measuring the unstimulated or stimulated saliva flow rate |
| 3. | Schirmer's test: This test measures the amount of saliva produced in a specific time. |
| 4. | Questionnaires: Xerostomia Inventory, Oral Health Impact Profile (OHIP), and the Oral Mucosal Dryness Scale (OMDS) are some of the questionnaires |
| 5. | Clinical examination: Physical examination of the mouth, including an evaluation of the salivary flow and oral mucosa for signs of dryness, such as dry and cracked lips, a dry tongue, and a lack of saliva in the mouth. |
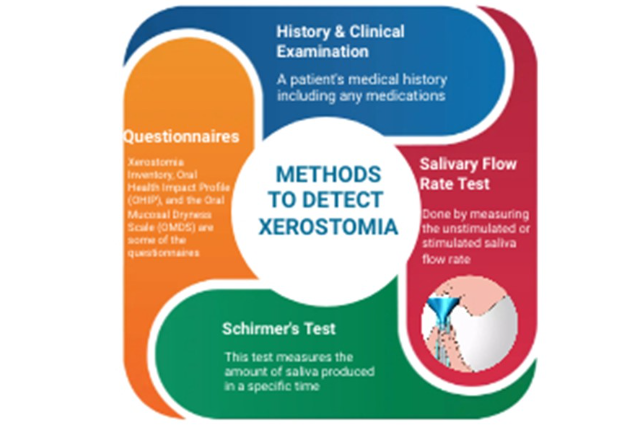
Figure 4A: Methods to Detect Xerostomia
Treatment/management
To improve oral health and prevent secondary infections, it is crucial to treat xerostomia. This involves educating the patient, taking preventative measures, providing symptomatic relief, using systemic and topical salivary stimulants, and implementing regenerative and gene therapies.31
Patient Education:
Xerostomia has a significant impact on both a patient's oral health and mental well-being, so educating them on the condition is essential to improve their quality of life. The patient should be informed of the consequences of xerostomia and instructed to drink water regularly to stay hydrated, limit their consumption of caffeine and alcohol, attend regular dental check-ups, and engage in preventive dental care such as using fluoridated trays, drinking fluoridated tap water, and using fluoridated mouthwash to prevent dental caries, candidiasis, and other oral complications.19
Prevention:
For xerostomia patients, it is recommended to increase the frequency of dental visits to every three to four months, instead of the typical six-month intervals. This is due to the increased risk of complications from reduced salivary flow, such as dental caries and oral candidiasis. To prevent these issues, regular radiographs, fluoride treatments, strict oral hygiene practices, and a low-sugar diet are recommended.19 The most effective method for preventing rampant caries caused by hyposalivation is the daily use of neutral pH sodium fluoride.32
Preventive solutions, such as fluorides and remineralizing agents, are available in various forms including varnishes, toothpaste, gels, and rinses, and can be used with or without applicator trays. It is preferred to use drugs with fewer side effects for xerostomia instead of those specifically associated with the condition. For instance, serotonin-specific reuptake inhibitors have been reported to cause less xerostomia compared to tricyclic antidepressants. Recent advancements in preventive therapy include relocating the salivary gland out of the radiation field.33
Symptomatic Treatment:
Saliva is a complex fluid with various components, each serving a specific purpose. For xerostomia treatment, patients can use water, artificial saliva, or glycerine.
Water is the most common symptomatic treatment. Artificial saliva can be made from ingredients such as mucin, carboxymethylcellulose, xanthan gum, hydroxyethylcellulose, linseed oil, or polyethylene oxide. Mucin, being a component of saliva, is the most well-tolerated by patients and has a longer-lasting effect compared to carboxymethylcellulose. Mucin-based artificial saliva is derived from porcine gastric mucosa, while carboxymethylcellulose-based artificial saliva has a sticky appearance that can irritate the underlying mucosa. Neither type is associated with any systemic side effects.
Artificial saliva is available in various forms such as lozenges, sprays, mouth rinses, gels, oils, chewing gums, or toothpaste, and can be used as swab sticks or added to denture reservoirs.34
Treatment with Systemic and Topical Salivary Stimulants
To enhance the production of saliva, there are two main types of salivary stimulants: those that stimulate receptors in the mouth and those that act directly on the parasympathetic nervous system. (Figure 5). The latter type is represented by pilocarpine, a cholinergic agent that increases saliva production by activating muscarinic receptors on exocrine glands. Pilocarpine is used to treat drug-induced, radiation-induced, and autoimmune-related xerostomia, as well as salivary gland dysfunction. The typical starting dose is 5 mg, taken three times daily, and can be increased to 30 mg per day if well-tolerated. The onset of action is 30 minutes and lasts for 4 hours. The most common side effect is sweating, while other potential side effects include gastrointestinal disturbances, nausea, urinary frequency, and vasodilation. It should not be used by patients with conditions such as asthma, heart disease, Parkinson's disease, or certain eye and urinary disorders.16,35
Other Parasympathomimetics
Cevimeline is another option for the treatment of xerostomia with fewer side effects compared to pilocarpine. It is recommended to take a dose of 30 mg three times a day, and it has a long-lasting effect. The most common side effect is dyspepsia. Other drugs, such as choline esters (bethanechol, neostigmine, distigmine), yohimbine, nicotinic acid, and malic acid, have also shown positive results in treating xerostomia.36
Herbal remedies, including jaborandi, betel nut, Iceland moss, and Longo Vital, can also stimulate salivary secretion.37
Intraoral topical salivary stimulants
Topical salivary stimulants that are used inside the mouth, such as lozenges, gum, jelly, sprays, mouthwashes, and toothpaste, are a common way to treat xerostomia. These products stimulate saliva production and keep the mouth hydrated through mechanical stimulation. Some of these topical stimulants may also contain components to prevent tooth decay and fungal infections, like fluoride, Xylitol, chlorhexidine, and calcium phosphate. Clinical trials have shown that lozenges containing mucin are more effective in treating xerostomia compared to a placebo.38
Other topical products, such as toothpaste, mouth rinse, spray, and gel, containing olive oil, betaine, and xylitol, may be effective in treating xerostomia caused by medication.39 Additionally, a non-invasive electrical stimulation system known as transcutaneous electrical nerve stimulation (TENS) has been shown to be effective in improving xerostomia and hyposalivation in patients with Diabetes Mellitus and postmenopausal conditions.40,41
Other treatments for xerostomia include the use of intraoral appliances like the Saliwell Crown device, which has been found to effectively reduce dry mouth symptoms and increase saliva production.42 Acupuncture may also help alleviate xerostomia and radiation-induced dry mouth. Additionally, amifostine, a cytoprotective agent, can minimize tissue damage caused by radiation therapy and decrease the risk of radiation-induced xerostomia.43,44 Finally, low-level laser therapy using infrared light of 904nm on the salivary glands has been found to be both stimulating and regenerative in nature in the treatment of xerostomia.45
Glandular regeneration and gene therapy
Stem cell therapy holds promise in the treatment of xerostomia caused by radiation-induced damage to salivary glands. This therapy aims to repair the damaged glands at a cellular level, with bone marrow stem cells, adipose tissue-derived stromal cells, and dental pulp cells being tested as forms of treatment for hyposalivation. Gene therapy, which involves the injection of a vector with genetic information into the tissue to achieve a beneficial change, has also shown potential in the treatment of xerostomia.31 In phase I/II study by Baum et al., an increase in saliva flow rate was seen from the targeted parotid gland. Gene therapy was previously used to treat congenital genetic disorders, but its principles are now applied to both acquired and inherited disorders.46

Figure 5: Treatment of Xerostomia
Differential Diagnosis
Xerostomia, also known as dry mouth, is a condition characterized by a decreased flow of saliva. Differential diagnosis of xerostomia includes:47
- Medications: Many medications, such as antidepressants, antihistamines, and diuretics, can cause dry mouth as a side effect.
- Sjogren's Syndrome: This is an autoimmune disorder that can cause dry mouth and dry eyes.
- Radiotherapy: Radiation therapy to the head and neck can cause damage to the salivary glands, leading to dry mouth.
- Dehydration: Not drinking enough fluids can cause dry mouth.
- Neurological disorders: Certain neurological disorders, such as Parkinson's disease and Alzheimer's disease, can cause dry mouth.
- Infections: Certain infections, such as HIV, can cause dry mouth.
- Smoking and Alcohol use: Smoking and heavy alcohol use can also cause dry mouth.
- Lifestyle factors: such as stress and anxiety can also cause dry mouth.
Prognosis
The prognosis for xerostomia (dry mouth) varies depending on the underlying cause. In some cases, the condition may be temporary and reversible, while in others it may be chronic and irreversible. Treatment options such as artificial saliva, saliva substitutes, and medications can help alleviate symptoms and improve quality of life. However, if the cause of xerostomia is a side effect of a medication or a result of a chronic condition such as Sjogren's syndrome, the condition may be managed but not cured. Regular dental check-ups and good oral hygiene practices can also help prevent complications associated with xerostomia.
Complications:
Xerostomia, or dry mouth, can lead to a number of complications including:
- Increased risk of dental cavities: Saliva plays an important role in neutralizing acids produced by bacteria in the mouth, which can lead to tooth decay. Without enough saliva, the risk of cavities increases.
- Difficulty swallowing: Xerostomia can make it difficult to swallow food and liquids, which can lead to malnutrition and dehydration.
- Sore throat or hoarseness: Dryness in the mouth and throat can cause irritation and soreness, making it difficult to speak or swallow.
- Bad breath: Without enough saliva, bacteria can thrive in the mouth, leading to bad breath.
- Increased risk of infection: Saliva helps to flush out bacteria and other harmful organisms from the mouth, making it harder for them to infect the body.
- Dry eyes and skin: Xerostomia can also affect the production of tears and the moisture of the skin, leading to dryness and irritation.
- Difficulty wearing dentures: Xerostomia can make it difficult to wear dentures as they may not fit properly and can cause discomfort.
- Gum disease: Saliva also helps keep the mouth clean and free of bacteria, so a dry mouth can increase the risk of gum disease.
- Changes in taste: A dry mouth can affect the sense of taste and make food less palatable.
- Difficulty speaking: A dry mouth can make it difficult to speak clearly.
- Psychological effects: Xerostomia can cause anxiety, depression, and reduced quality of life due to the associated complications. (Figure 5)
It's important to manage xerostomia, as it can lead to serious oral health problems if left untreated.
Figure 6: Complications of Xerostomia
Conclusion:
In conclusion, xerostomia is a common condition characterized by dry mouth and reduced saliva flow. There are various causes of xerostomia, including medication use, radiation therapy, and certain medical conditions. To manage xerostomia, there are a variety of treatment options available, including behavioral modifications, saliva substitutes, intraoral topical stimulants, and various therapies. Additionally, glandular regeneration and gene therapy are promising new treatments for patients with radiation-induced xerostomia. The best treatment for an individual will depend on the underlying cause of their xerostomia, as well as their personal preferences and needs.
. . .
References:
- Nederfors T. Xerostomia and hyposalivation. Adv Dent Res. 2000 Dec;14:48-56
- Orellana, M. F., Lagravère, M. O., Boychuk, D. G., Major, P. W., Flores-Mir, C., & Ortho, C. Prevalence of Xerostomia in Population-based Samples: A Systematic Review. Journal of Public Health Dentistry,2006; 66(2), 152–158. doi:10.1111/j.1752-7325.2006.tb02572.x
- Fox RI, Stern M, Michelson P. Update in Sjogren syndrome. Curr Opin Rheum 2000;12:391–398
- https://www.ada.org/resources/research/science-and-research-institute/oral-health-topics/xerostomia
- Pujol T, Coma M, Pujol M, Postigo P. Prevalencia de xerostomía en la población general [Prevalence of xerostomia in the general population]. Aten Primaria. 1998 ;21(4):225-8. Spanish. PMID: 9607250.
- Pinto VL, Fustinoni SM, Nazário ACP, Facina G, Elias S. Prevalence of xerostomia in women during breast cancer chemotherapy. Rev Bras Enferm. 2020;73(Suppl 4):e20190785. doi: http://dx.doi.org/10.1590/0034-7167-2019-0785
- https://www.merckmanuals.com/professional/dental-disorders/symptoms-of-dental-and-oral-disorders/xerostomia
- Waterhouse. J. P.. Chisholm. D. M., Winter, R. B.. Patel. M.. and Yale, R. S.- Replacement of functional parenchymal cells by fat and connective tissue in human submandibular salivary glands An age-related change J. Oral Path. 1973; 2: I. 16-27,
- Scott, J.A morphometric study of age changes in the histology of the ducts of human submandibular salivary glands. Arch. Oral Biol. 1977; 22: 4. 243-249.
- FelipeFredes, C. “Manejo actual de la xerostomía.”. Rev. Otorrinolaringol. Cir. Cabeza Cuello. 2016;vol.76 no.2 Santiago ago.
- López-López, J., Jané Salas, E., & Chimenos Küstner, E. (2014). Pronóstico y tratamiento de la boca seca. Revisión sistemática. Medicina Clínica, 2013;142(3), 119–124.
- Sreebny LM. Vissink A. Dry mouth: The Malevolent Symptom: A Clinical Guide.2021.Chapter 2.Dry Mouth: a multifacetedbdiagnpostic dilemma. 2.2: Symptoms and semiotics: page:52-63.Willey-Blackwel publisher.
- Mortazavi H, Baharvand M, Movahhedian A, Mohammadi M, Khodadoustan A. Xerostomia Due to Systemic Disease: A Review of 20 Conditions and Mechanisms. Ann Med Health Sci Res 2014; 4(4): 503-10.
- Hanchanale S, Adkinson L, Daniel S, Fleming M, Oxberry Sg. Systematic literature review: xerostomia in advanced cancer patients. Support Care Cancer 2015; 23(3): 881-8.
- Montgomery-Cranny J, Hodgson T, Hegarty Am. Etiology and management of xerostomia and salivary gland hypofunction. Br J Hosp Med (Lond) 2014; 75(9): 509-10, 511-4.
- Visvanathan V, Nix P. Managing the patient presenting with xerostomia: a review. Int J Clin Pract. 2010 Feb;64(3):404-7. doi: 10.1111/j.1742-1241.2009.02132.x. Epub 2009 Oct 10. PMID: 19817913.
- Mason DK, Chisholm DM: Changes in salivary secretion and composition in disease, in Salivary Glands in Health and Disease. Philadelphia, WB Saunders, 1975, pp. 119-137
- Hong Wu, M.D., M.S.1,2, Jennifer Yacub Martin, M.D.1 and Dian Wang, M.D., Ph.D. Xerostomia: Causes, Prevention and Management. In: Horizons in Cancer Research. Volume 55 ISBN: 978-1-63463-228-7. Chapter 4. 101-121.
- Napeñas, J.J., Brennan, M.T. & Fox, P.C. Diagnosis and treatment of xerostomia (dry mouth). Odontology .2013;97, 76–83.https://doi.org/10.1007/s10266-008-0099-7
- Osailan S, Pramanik R, Shirodaria S, Challacombe SJ, Proctor GB. Investigating the relationship between hyposalivation and mucosal wetness. Oral Dis. 2011;17(1):109–114.
- Löfgren CD, Wickström C, Sonesson M, Lagunas PT, Christersson C. A systematic review of methods to diagnose oral dryness and salivary gland function. BMC Oral Health. 2012;12:29.
- Navazesh, M. Methods for Collecting Saliva. Annals of the New York Academy of Sciences, 694(1 Saliva as a D), 1993; 72–77. doi:10.1111/j.1749-6632.1993.tb18343.x
- Dost F, Farah CS. Stimulating the discussion on saliva substitutes: A clinical perspective. Australian Dental Journal. 2013;58:11-17. DOI: 10.1111/adj.12023
- Ugga L, Ravanelli M, Pallottino AA, Farina D, Maroldi R. Diagnostic work-up in obstructive and inflammatory salivary gland disorders. Acta Otorhinolaryngologica Italica. 2017;37:83- 93. DOI: 10.14639/0392-100X-1597
- Ship JA, Fox PC, Michalek JE, Cummins MJ, Richards AB. Treatment of primary Sjogren's syndrome with low-dose natural human interferon-alpha administered by the oral mucosal route: A phase II clinical trial. IFN Protocol Study Group. Journal of Interferon & Cytokine Research. 1999;19:943-951. DOI: 10.1089/107999099313497
- Bascones-Martinez A, Munoz-Corcuera M, Bascones-Ilundain C. Side effects of drugs on the oral cavity. Medicina Clínica (Barcelona). 2015;144:126-131. DOI: 10.1016/j.medcli. 2014.01.025
- Dodds MW, Johnson DA, Yeh CK. Health benefits of saliva: A review. Journal of Dentistry. 2005;33:223-233. DOI: 10.1016/j.jdent.2004.10.009
- Zero DT, Brennan MT, Daniels TE, Papas A, Stewart C, Pinto A, Al-Hashimi I, Navazesh M, Rhodus N, Sciubba J, Singh M, AJ W, Frantsve-Hawley J, Tracy S, Fox PC, Ford TL, Cohen S, Vivino FB, Hammitt KM. Clinical practice guidelines for oral management of Sjogren disease: Dental caries prevention. Journal of the American Dental Association. 2016;147:295-305. DOI: 10.1016/j.adaj.2015.11.008
- Saavedra AJRM, Bozo MI, Ríos HM. Estudio de confiabilidad de la prueba de sialometría para flujo no estimulado en sujetos adultos clínicamente sanos. Revista Clínica de Periodoncia, Implantología y Rehabilitación Oral. 2013;6:25-28
- Daniels TE. Labial salivary gland biopsy in Sjögren’s syndrome. Arthritis Rheum 1984;27:147–56.
- Escobar, Alejandro and Juan Aitken-Saavedra. “Xerostomia: An Update of Causes and Treatments.” Salivary Glands - New Approaches in Diagnostics and Treatment (2019): n. pag. 15-35. http://dx.doi.org/10.5772/intechopen.72307
- Shiboski CH, Hodgson TA, Ship JA, Schiodt M. Management of salivary hypofunction during and after radiotherapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;103:S66. e1–19.
- Jha N, Seikaly H, Harris J, Williams D, Liu R, McGaw T, Hofmann H, Robinson D,Hanson J, Barnaby P. Prevention of Radiation Induced Xerostomia by Surgical Transfer of Submandibular Salivary Gland Into the Submental Space. 2003. Available from: http:// www.ncbi.nlm.nih.gov/pubmed/12742268
- Davies, A. (1997). The management of xerostomia: a review. European Journal of Cancer Care, 6(3), 209–214. doi:10.1046/j.1365-2354.1997.00036.x
- Gotrick B, Akerman S, Ericson D, Torstenson R, Tobin G. Oral pilocarpine for treatment of opioid-induced oral dryness in healthy adults. Journal of Dental Research. 2004;83:393- 397. DOI: 10.1177/154405910408300508
- Grisius MM. Salivary gland dysfunction: A review of systemic therapies. Oral Surgery,Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics. 2001;92:156-162. DOI:10.1067/moe.2001.116601
- Miranda-Rius J, Brunet-Llobet L, Lahor-Soler E, Farre M. Salivary secretory disorders,inducing drugs, and clinical management. International Journal of Medical Sciences. 2015;12:811-824. DOI: 10.7150/ijms.12912
- Gravenmade EJ, Vissink A. Mucin-containing lozenges in the treatment of intraoral problems associated with Sjögren’s syndrome. A doubleblind crossover study in 42 patients. Oral Surg Oral Med Oral Pathol. 1993;75(4):466–471.
- Ship JA, McCutcheon JA, Spivakovsky S, Kerr AR. Safety and effectiveness of topical dry mouth products containing olive oil, betaine, and xylitol in reducing xerostomia for polypharmacy-induced dry mouth. J Oral Rehabil. 2007;34(10):724–732.
- Dyasnoor S, Kamath S, Khader NFA. Effectiveness of electrostimulation on whole salivary flow among patients with type 2 diabetes mellitus. The Permanente Journal. 2017;21:15-164. DOI: 10.7812/TPP/15-164
- Konidena A, Sharma D, Puri G, Dixit A, Jatti D, Gupta R. Effect of TENS on stimulation of saliva in postmenopausal women with or without oral dryness—An interventional study. Journal of Oral Biology and Craniofacial Research. 2016;6:S44-S50. DOI: 10.1016/j.jobcr.2016.01.004
- Alajbeg I, Falcão DP, Tran SD, et al. Intraoral electrostimulator for xerostomia relief: a long-term, multicenter, open-label, uncontrolled, clinical trial. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113(6):773–781
- Blom M, Dawidson I, Angmar-Månsson B. The effect of acupuncture on salivary flow rates in patients with xerostomia. Oral Surg Oral Med Oral Pathol. 1992;73(3):293–298
- Koukourakis MI. Amifostine in clinical oncology. Current use and future implications. Anticancer Drugs 2002; 13: 181–209
- Lončar M, Mravak-Stipetić M, Risović D. The effect of low-level lasertherapy on salivary glands in patients with xerostomia. Photomed Laser Surg. 2011; 29(3):171-5.
- Baum BJ, Alevizos I, Zheng C, Cotrim AP, Liu S, McCullagh L, Goldsmith CM, Burbelo PD, Citrin DE, Mitchell JB, Nottingham LK, Rudy SF, Van Waes C, Whatley MA, Brahim JS, Chiorini JA, Danielides S, Turner RJ, Patronas NJ, Chen CC, Nikolov NP, Illei GG. Early responses to adenoviral-mediated transfer of the aquaporin-1 cDNA for radiationinduced salivary hypofunction. Proceedings of the National Academy of Sciences of the United States of America. 2012;109:19403-19407. DOI: 10.1073/pnas.1210662109
- K. E. Murphy, "Xerostomia: causes, consequences, and management," Journal of the American Pharmacists Association, vol. 45, pp. e41-e52, 2005.
