ABSTRACT
This paper analyses the role of Aam Aadmi Mohalla Clinics in improving primary healthcare in India and how they cater to the demand of the patients. These clinics provide basic services in underserved areas in a receptive manner and free of cost. This scheme has garnered much recognition worldwide and also by other Indian states that they plan to adopt a similar healthcare structure to improve the health status. This article covers the gender disparity prevalent in patients at these clinics and the factors that influence the satisfaction of patients. The paper also establishes how these clinics have made primary healthcare affordable by reducing the cost burden on patients. It also lists various ways of improving these clinics.
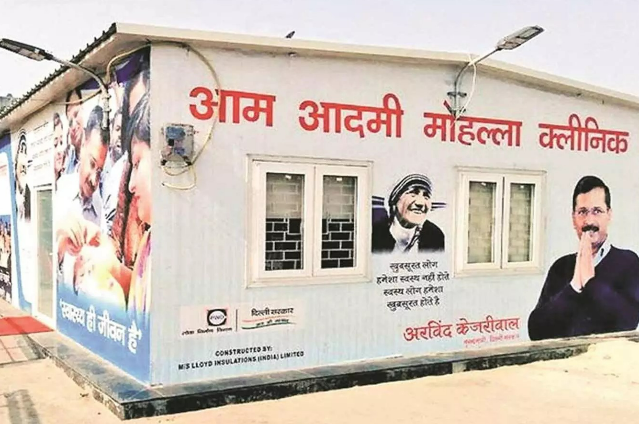
INTRODUCTION
“Healthy citizens are the greatest asset any country can have.” - Winston Churchill.
Health is an important factor contributing to the economic progress of any nation. A healthy population lives longer, is more productive and acts as a catalyst in the economic growth. It is also central to the well being and happiness of people and society. Mohalla Clinics is a new concept in primary healthcare system undertaken by the Government of India. They provide an assured package of services with the aim of making basic healthcare more accessible. The services provided are free of cost and they make it all affordable by reducing indirect costs like travel since the clinics are set up in residential areas. Over the years, this system has received global recognition. Kofi Annan, former secretary general of UN expressed that the project could be a model for all Indian states “embarking on the universal healthcare journey.”
The lack of primary health-care units had led to overcrowding in government hospitals which in turn led to delay in treatment of patients. Mohalla clinics cater to these problems hence ensuring quicker and cost effective treatment. There are currently 158 such clinics in rented premises and porta-cabins that are operational Monday to Friday from 8 am to 2pm. Each clinic has four employees - a doctor, a nurse, a pharmacist and a technician. According to the GoI website, they provide 109 types of essential medicines, and are equipped to conduct over 200 tests and initial diagnosis. Apart from providing treatment for common illnesses like fever, diarrhoea etc., first aid for injuries and burns, antenatal and postnatal care for pregnant women, are also provided. They also aim to spread preventive education and awareness among the people.
BACKGROUND
The healthcare system prior to the introduction of Mohalla Clinics, included primary urban health centres (PUHCs) and dispensaries run by the central and state government. These centers were equipped with basic laboratory services and provided services like immunization, reproductive healthcare, general OPDs and referrals. They also carried out outreach programmes in underserved localities in association with other healthcare organizations, particularly concerned with maternal and child health.
However, despite these healthcare centres, there was a lack of availability of primary healthcare since these centres were not uniformly spread across all areas /localities and faced the problem of severe overcrowding as they were significantly understaffed. There was a pressing need to improve the healthcare system and strengthen the primary healthcare as it is one of the basic human needs.
The Government of Delhi in 2015 started the Aam Aadmi Mohalla Clinics (AAMC) with the aim of tackling this problem of overcrowding and understaffing. They reorganised the healthcare system and divided it into four levels which are as follows:
- Aam Aadmi Mohalla Clinic for primary health care.
- Multi Speciality Poly Clinic for secondary health care in the form of OPD consultation by specialist doctors including diagnostics. (Conversion of dispensaries into polyclinics)
- Multi-Speciality Hospital for IPD care (earlier called Secondary Level Hospital)
- Super-Speciality Hospital earlier called Tertiary Level Hospital.
According to this paper, since the government does not have to pay doctors salaries and their wages are tied to the number of patients they meet, problems such as doctors absenting themselves from work and arriving late do not arise. But a number of problems were faced by patients in regard to these areas as doctors sorted to over invoicing of patients and reduced time per patient, to make more profit. Also, the results of the tests conducted were also questionable as some claimed them to provide wrong reports. Another article by Kuruvilla (2017), critiqued the clinics on multiple fronts starting with how the system of remuneration linked with the number of patients has lead to doctors inflating their bills. He also agreed with the problem of the clinics focussing solely on curative services and not prevention.
Why do we see this articular proportion?
I. Medicines provided at Mohalla Clinics are completely free:
This implies that people who earlier might have waited a few days to visit a doctor/chemist and buy costly medicines may now simply visit the clinic at the first sign of sickness. This improves the standard of health of the people who otherwise find it hard to afford expensive healthcare.
II. Time spent per patient is low in these clinics majorly because of two reasons:
a) Crowded clinics - When the doctors are attending to a big crowd of patients, the time per patient is reduced and patients could not classify it as getting a proper check up but only a prescription of medicines. The doctors were done with each patient in 5-7 minutes (including registration);
b) Ill-informed patients - Most patients visiting these clinics are not well informed about medical complexities. Hence, the doctors might not find it fruitful to explain the sickness/medicines in detail to the patients and rather prefer to move on to the next patient.
III. Patients suffering from a chronic or prolonged disease already possess a subscription of medicines provided to them by the polyclinic/hospital:
So they can simply visit a Mohalla Clinic to pick up their medicines, if those medicines are dispensed by the clinic.
IV. A number of patients who are diagnosed at the polyclinics/hospitals are referred to the AAMCs for basic tests and medicines:
(ex: blood test, thyroid and other common tests). This also results in a lower count of check-ups since the patient has already been checked by the doctor at a polyclinic and the relevant test has been prescribed. The AAMC only needs to carry out the test. Also, According to NSSO data for the year 2014, out of the total medical expenditure, around 72% in rural and 68% in urban areas was made for purchasing ‘medicine’ for non- hospitalised treatment. Along with this, the data collected from our community revealed that people’s private expenditure varied from one locality to another. In some areas people incurred expenditure ranging from 100-500 rupees, and in more well off localities this range was around 500- 1000 rupees. Since medicine comprises of a very high proportion of expenditure incurred and the report shows that most patients come to collect their medicines alone which are completely free at the AAMC, it should lead to a contraction in the healthcare expenditure.
HOW CAN MOHALLA CLINICS BE STRENGTHENED?
- Female patients have expressed the requirement of a female doctor, if not a gynaecologist, as they would be more comfortable in talking to a woman. Also, the proportion of women is high in the clinic’s patient base. Hence, there should be more female doctors appointed.
- Most of the rented accommodations were two room sets which failed to accommodate the excessive crowd in most clinics. The queues of patients extended till outside the clinics. There is a clear need for either an improvement in infrastructure or increasing the concentration of clinics in the localities.
- A system of monitoring the doctors, staff and the services provided should be put in place as to avoid wastage of resources and ensure professional behaviour. Parchi or token system should be started to ensure discipline among the patients waiting in queues.
- Ensuring cleanliness in and around the clinics and installing dustbins for patients to dispose bandages is an important step to make the clinics better.
- Some patients need to find public washrooms to give their stool tests, and some tend to vomit right outside the clinic. Hence, the facility of a washroom for patients is very essential.
- Complaint boxes should be installed as mentioned by the website so that patients can express any grievances.
- Postnatal and antenatal care for pregnant women as said by their website is not provided in any clinic and it would be a major benefit for the women living nearby these clinics if it were.
- These clinics can be used to spread awareness regarding sanitation and personal hygiene to the patients and promote prevention more than cure.
- The only information about the addresses of the clinics is available online or through word of mouth. Since most people don’t have access to internet, there should be more effort towards increasing awareness of the existence of these clinics.
CONCLUSION
“When I is replaced by We, even Illness becomes Wellness.” - Malcolm X, African-American Minister.
Our findings depict that Mohalla Clinics have been a great success in India and have been able to meet their aims to a large extent. The high level of satisfaction and analysis of various pull factors bolsters this initiative of the government and the expansion of this scheme would certainly benefit the community and help uplift the health status of people. The clinics provide all facilities completely free of cost, and travel expenses are negligible. This also brings down the cost burden of healthcare, which is otherwise quite high and distressing for the actual poor. However, looking at the bigger picture they lack some important features which could improve the condition and functioning of these clinics. By incorporating changes such as evening operating hours, more hygienic surroundings, washroom facility, better infrastructure, they could attract a larger patient base. People who currently do not visit the clinic for reasons that are stated by the respondents, may be willing to visit if such changes were made. Given the high proportion of women visiting these clinics that require the appointment of more female doctors, it validates how Mohalla Clinics could make themselves better by catering to the needs of such women and employing not only female doctors, but also gynaecologists. Their website also claims that the clinics provide prenatal and antenatal care for pregnant women. However, our findings reveals that no such facility is available. Appointing a gynaecologist, for specific days of the week, could go a long way in improving the health of all women in these localities. Mohalla Clinics appeal to most people because of the negligible cost of healthcare and an increase in the number of such clinics would make primary healthcare more accessible hence benefitting the underserved population who otherwise find it hard to afford healthcare.
. . .
END NOTES:
- NSSO Data (2014) – Health in India, NSS 71st round, Government of India, Ministry of Statistics and Programme Implementation, National Sample Survey Office. Website: mospi.nic.in (last accessed October 2018)
- Lahariya, Chandrakant. "Mohalla Clinics of Delhi, India: Could these become platform to strengthen primary healthcare?." Journal of family medicine and primary care 6, no. 1 (2017)
- Bhandari, Aditya, Ishan Bhardwaj, and Sunidhi Sawhney. "Quality and Accessibility of Government Hospitals and Mohalla Clinics." DELHI CITIZENS’: 94.
- Kuruvilla, Benny. "Against the grain: New pathways for essential services in India." Reclaiming Public Services (2017).
- Delhi Human Development Report(2013) www.delhi.gov.in
- Delhi Government website - www.delhi.gov.in (last accessed October 2018)
- Aam Aadmi Mohalla Clinic Website – aamaadmiparty.org (last accessed October 2018)