Infertility, while not life-threatening still inflicts significant emotional distress and trauma on affected couples which is a pain best articulated by those experiencing it. Although detailed statistics on infertility in India are lacking. A multinational study by the WHO (1988) indicates that the prevalence of infertility in India ranges from 10% to 15%. Considering India's population of around 1 billion there are approximately 250 million people who might be attempting to start a family at any given time. Based on WHO estimates, this suggests that 13 to 19 million couples in India could be infertile at any given moment.
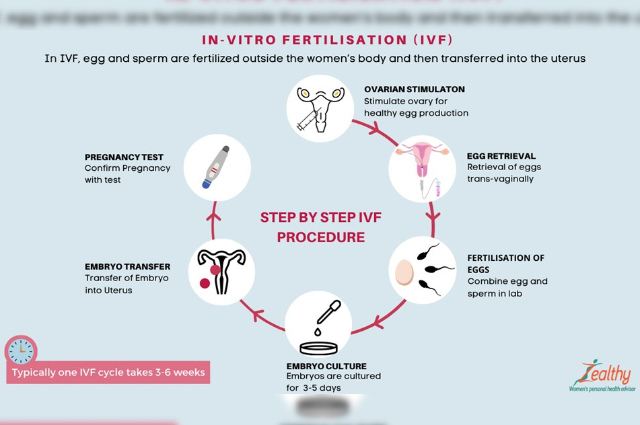
The International Conference on Population and Development (ICPD) Programme of Action includes the prevention and treatment of infertility as part of primary healthcare. Many infertility cases, such as those caused by reproductive tract infections and genital tuberculosis are preventable and treatable. However, about 8% of infertile couples require advanced medical interventions like Assisted Reproductive Technologies (ART) procedures such as In Vitro Fertilization (IVF) and Intracytoplasmic Sperm Injection (ICSI). These treatments are costly and mostly high-priced for the majority of Indians. Furthermore, ART demands significant technical skill with expensive infrastructure and even under the finest conditions the success rate of these procedures is below 30%.
In India, infertility carries deep societal implications. The growing use of ART requires stringent measures to ensure the safety and prevent the misuse of these technologies. Internationally, scientific organizations like the ASRM (American Society for Reproductive Medicine), ESHRE ( European Society of Human Reproduction and Embryology ) and IFFS ( International Federation of Fertility Societies ) have developed guidelines to ensure the safe and ethical practice of ART. Additionally, countries such as Australia, UK , and the USA along with the European Union have established authorisation and regulatory frameworks to oversee infertility clinics. This global model emphasizes the importance of implementing similar safeguards in India to protect and support couples on their journey towards parenthood.
The Vital Role of Egg Freezing in Modern Reproductive Health
Cryopreservation has long been a cornerstone of assisted reproductive technology. Since the first successful preservation of sperm in 1953 and embryos in the 1980s, these techniques have become standard practice. Notably, Dr. Christopher Chen of Singapore achieved the world’s first pregnancy using previously frozen oocytes in 1986. Today, egg freezing serves three primary groups of women such as those diagnosed with cancer who have yet to begin chemotherapy or radiotherapy, those undergoing assisted reproductive treatments who cannot or choose not to freeze embryos due to legal or personal reasons and those who wish to delay childbearing for personal or medical reasons.
Each year, over 50,000 women of reproductive age in the USA are diagnosed with cancer. This number is rising in developing countries due to aging populations and the adoption of lifestyles associated with cancer such as smoking, inactivity and unhealthy diets. Chemotherapy and radiotherapy can severely damage oocytes, leaving women with few living eggs. Egg freezing offers these women the hope of future parenthood by preserving their eggs before treatment begins.
For individuals undergoing in vitro fertilization (IVF) who oppose embryo freezing on religious or ethical grounds, egg freezing provides a valuable alternative. It allows for fertilizing only the number of eggs needed for the IVF process and freezing any remaining unfertilized eggs. This approach avoids the ethical dilemmas associated with the disposal of unused embryos.
Additionally, egg freezing is beneficial for women who wish to delay childbearing due to educational, career or other personal reasons. Freezing eggs at a younger age can secure the possibility of future pregnancies. Women with a family history of early menopause may also seek fertility preservation by ensuring they have a supply of living eggs even if they experience early depletion.
Social Egg Freezing: A guide for women considering Fertility Preservation
What is social egg freezing?
Social egg freezing allows women to preserve their fertility by freezing their eggs for future use. This process involves extracting mature eggs and freezing them at a very low temperature. After this storing them until the woman decides to get pregnant. Later, the eggs can be utilized through fertilization with sperm through in vitro fertilization (IVF) and implanted in the uterus as embryos for a successful pregnancy. Social egg freezing differs from medically necessary egg freezing as it's done for non-medical reasons such as delaying childbearing for personal, professional or financial reasons.
How is social egg-freezing done?
The egg-freezing process involves several steps:
- Counselling & Ovarian Reserve Testing: A woman considering social egg freezing will undergo counselling to understand the success rates and potential risks. Doctors will also perform tests like Anti-Müllerian Hormone (AMH) and Antral Follicle Count (AFC) to assess the potential number of eggs that can be retrieved.
- Egg Stimulation and Retrieval: Through hormone injections, the ovaries are stimulated to produce multiple eggs at once. These eggs are then retrieved using a minor surgical procedure called transvaginal oocyte retrieval.
- Freezing and Storage: The retrieved eggs are frozen at subzero temperatures using a process called vitrification. These frozen eggs can then be stored for many years until the woman is ready to use them.
Benefits of Social Egg Freezing
Social egg freezing offers several advantages for women who may want to delay pregnancy:
- Preserve Fertility Potential: As women age, their fertility naturally declines. Social egg freezing allows women to preserve their eggs when they are young and healthy by potentially increasing their chances of a successful pregnancy later in life.
- Greater Control Over Family Planning: Social egg freezing empowers women to delay childbearing for personal or professional reasons without compromising their future fertility options.
- Reduced Risk of Chromosomal Abnormalities: Eggs from younger women have a lower risk of chromosomal abnormalities compared to eggs from older women. This reduces the chances of having a child with a genetic condition.
- Alternative to Embryo Freezing: For women who have ethical concerns about embryo freezing, social egg freezing offers a way to preserve their fertility without creating embryos.
Why is Fertility Declining Among Indian Women?
India is experiencing a significant decline in female fertility, particularly in urban areas. This trend can be attributed to several key factors:
- Later Marriage and Career Focus: The average age of marriage for women in India is rising. This overlaps with a growing emphasis on education and career building, especially in urban areas. Women are dedicating their twenties and thirties to professional careers and that’s leading to delaying marriage and childbearing.
- Shifting Priorities: Economic and social changes have contributed to a shift in priorities for many Indian couples. They may choose to delay parenthood for financial stability or the desire to find a compatible partner.
- Biological Factors: Studies suggest that regional background may play a role. Women from the Indian subcontinent may have a lower ovarian reserve compared to women from Western countries. This can translate to a biological decline in fertility at a younger age.
- Reduced peak fertility period: The most fertile years for women are generally considered to be in their twenties and early thirties. With later childbearing, couples often find themselves attempting to conceive after this period has narrowed which leads to a decrease in pregnancy success rates.
The Promise of Vitrified Eggs in IVF: Similar Success Rates and Offering Options
The ability to achieve a live birth through In Vitro Fertilization (IVF) is no longer dependent solely on fresh eggs. Extensive research has shown that vitrified or frozen eggs offer similar success rates compared to fresh eggs in IVF treatment. This part explores the factors influencing pregnancy outcomes with frozen eggs and the potential benefits this technology offers to a wider range of patients seeking fertility assistance.
The key determinants for a successful pregnancy using frozen eggs lie in two crucial aspects: the woman's age at the time of egg freezing and the number of eggs retrieved. As women age, their ovarian reserve diminishes which leads to a decline in the quantity and quality of available eggs. A younger woman (early thirties) might have a significantly higher number of eggs (15-20) suitable for freezing after stimulation compared to women in their late thirties or forties. Additionally, the risk of chromosomal abnormalities in eggs increases with age.
The success of IVF with frozen eggs depends on the survival of these eggs throughout the process. Not all retrieved eggs are suitable for freezing and some may not survive the vitrification and melting procedures. Similarly, not all frozen eggs will fertilize or develop into embryos. Finally, even transferred embryos may not implant or may even result in a miscarriage.
Despite these potential losses, current research suggests that vitrified oocytes and a rapid freezing technique offer superior results compared to the older slow-freezing methods. Moreover, studies indicate that vitrified eggs may achieve outcomes comparable to fresh eggs for specific patient groups.
This technology unlocks possibilities for a broader range of individuals seeking fertility solutions. Patients facing potential infertility due to age-related decline, medical conditions or those participating in egg donation programs can benefit from cryopreserved oocytes. Additionally, couples facing challenges with sperm production during IVF or those with ethical or legal concerns regarding embryo freezing can find an alternative path to parenthood through frozen eggs.
Furthermore, vitrification offers a solution for those with moral objections to embryo freezing. By freezing eggs before fertilization, these individuals can pursue IVF while observing their views. Vitrification of eggs has revolutionized fertility treatments. With success rates comparable to fresh eggs, this technology empowers individuals and couples to make informed choices about their family planning. By offering a safe and effective option for protective fertility, vitrification removes age and certain medical concerns as barriers to achieving parenthood.
Ovarian Function, Fertility and Age

Egg Development and Aging
During a woman's reproductive years, the ovaries contain hundreds of thousands of unfertilized eggs. Over several weeks, multiple eggs begin to develop in waves but most stop growth while one mature egg continues to develop and is released in each cycle. As women age, the number of eggs available for maturation decreases and by around age 50, no healthy eggs remain to be alive. Women's fertility rate is mostly developed in their 20s and early 30s when the ovaries have a substantial number of healthy eggs. In the 10-15 years leading up to menopause, ovarian function deteriorates despite regular ovulatory cycles, particularly affecting women in their forties who face a diminished chance of producing a healthy pregnancy due to declining egg quality.
Technique: Hormonal Stimulation
To obtain eggs for freezing, women typically undergo hormonal stimulation over 10-12 days to mature a group of eggs. The number of eggs retrieved depends on individual circumstances; women under 35 with a normal ovarian reserve usually produce 10-15 eggs. Various stimulation techniques are available and most doctors select as per the suitable needs of patients. The stimulation medications are self-administered by pen injection with a tiny needle and patients are taught this procedure in an instructional session. These injections may cause slight bloating but most women can continue their normal activities until the day of egg recovery.
Procedure to Remove the Eggs
Egg retrieval is a minor procedure performed under restfulness. This will take about 15 to 20 minutes. The fertility specialist uses an ultrasound-guided probe with an attached needle to draw fluid and eggs from the ovary through the vaginal wall. Patients can usually go home with a companion about an hour after the procedure and are advised to rest for the remaining day.
Egg Freezing Procedure
In the IVF laboratory, eggs are frozen using vitrification which is a fast-freezing method. Eggs can be stored for many years without deterioration. When the woman is ready to use her eggs, they are defrosted, fertilized with sperm and then developed into embryos. A mature embryo or blastocyst is then transferred to the woman’s uterus that’s offering a chance of pregnancy.
Risks of Egg Freezing
Complications from Hormonal Stimulation
Egg freezing is generally safe but potential complications can arise from hormonal stimulation and the egg collection procedure. Hormone administration may slightly increase the risk of thrombosis (clots), so it's important to inform your doctor if you have a personal or family history of clots. Possible side effects include under or over-stimulation of the ovaries and rarely failure to obtain eggs. Complications from egg retrieval such as pelvic infections or trauma are uncommon.
Treatment-Related Complications
Further details about treatment-related complications are provided in the relevant consent form. Risks include the potential failure of eggs to survive defrosting, fertilising, developing into embryos or resulting in pregnancy after embryo transfer. Women should also consider other options, such as donor fertilization or using donor eggs in the future. Pregnancy in older women carries increased risks of complications like high blood pressure and gestational diabetes which are unrelated to egg age but related to the age of the woman carrying the pregnancy cycle.
Factors Impacting Egg Freezing
Egg freezing is a significant decision for many women and that’s influenced by a variety of factors. Understanding these can help in making informed choices about the process.
Age
The age of the woman is a critical factor in egg freezing. As women age, both the quality and quantity of their eggs decline. Therefore, it is recommended to freeze eggs at a younger age ideally between 25 and 35 years. This age range offers the best chances for successful egg preservation.
Associated Medical Conditions
Several medical conditions can adversely affect egg quality making it essential to be aware of them before undergoing egg freezing. Conditions such as endometriosis, genital tuberculosis, uncontrolled diabetes and various auto-immune disorders are significant factors. Being informed about these health issues is crucial as they can impact both the procedure and the quality of the frozen eggs.
Stimulation Protocols and Injections
Choosing the correct stimulation protocols and the appropriate injections along with the right dosages is vital for achieving optimal results in egg freezing. The selection of these protocols should be done carefully in consultation with a medical professional to ensure the best possible outcome.
Faulty Freezing Techniques
The choice of clinic plays a crucial role in the success of egg freezing. It is important to select a clinic that adheres to high standards in maintaining the IVF laboratory environment. Proper freezing techniques are essential for the safety and long-term storage of eggs by ensuring their feasibility when they are eventually used.
Skilled Technicians and Embryologists
The expertise of the medical team, particularly the embryologists is crucial for the success of the egg-freezing procedure. Skilled embryologists are necessary to handle the delicate process of egg retrieval and freezing by increasing the likelihood of successful preservation.
Some other risks Associated with Egg Freezing
While egg freezing is generally safe still it is not without risks. However, when performed by an experienced and skilled team such risks are rare. Some of the potential risks include:
- Poor Response to Stimulation Injections: Some women may not respond well to the injections that will be resulting in fewer eggs being retrieved.
- Ovarian Hyperstimulation Syndrome (OHSS): This condition can occur in young women with a good ovarian reserve, leading to swollen and painful ovaries.
- Procedure-Related Injuries: In rare cases, the egg retrieval process can cause injury to the urinary bladder, bowels or blood vessels.
Understanding these factors and potential risks can help women make informed decisions about egg freezing and that can ensure they approach the procedure with the best possible chance for success.
The Scope of Egg Freezing for Pre-Menopausal Women in India

Availability and Considerations
Egg freezing also known as oocyte cryopreservation is becoming more prevalent in India although it remains less widespread compared to some other countries. The effectiveness of egg freezing is influenced by several factors, including age, health, and reproductive history. Typically, women under the age of 35 have a higher success rate, while those over 38 may see reduced outcomes due to the natural decline in egg quality and quantity with age.
A key factor in determining the viability of egg freezing is the Anti-Mullerian Hormone (AMH) level, which provides an estimate of ovarian reserve. Younger women generally have higher AMH levels which correlate with a greater number of retrievable eggs and potentially better outcomes.
Cost of Egg Freezing in India
The cost of egg freezing in India ranges from INR 1,20,000 to INR 2,50,000, making it relatively affordable compared to international prices. This cost includes medications, the egg retrieval procedure and the initial year of storage. However, additional costs may arise from extended storage periods or further treatments. It's advisable to discuss financial aspects thoroughly with a fertility specialist as many clinics offer financial assistance and various financing options to make the procedure more accessible.
Age Limitations for Egg Freezing
Fertility declines significantly with age, especially after the mid-30s. Therefore, it is generally recommended to consider egg freezing at a younger age to maximize the chances of future pregnancy and minimize risks such as miscarriages, birth defects and chromosomal abnormalities. Consulting with a fertility specialist can help determine the optimal time for egg freezing based on individual health and reproductive goals.
Duration of Egg Storage
Eggs can be stored for long periods without significant degradation in quality with current data supporting storage for up to four years or more. However, the risks associated with pregnancy at an older age such as high blood pressure, diabetes and the need for a cesarean section should be considered. Additionally, many clinics impose age limits for using stored eggs to achieve pregnancy by emphasizing the importance of timely planning.
Potential Side Effects on Babies Conceived through Egg Freezing
Research indicates that babies conceived from frozen eggs generally have similar health outcomes to those conceived naturally or through fresh IVF cycles. Although assisted reproductive technologies are continually advancing, current studies have not found substantial evidence of specific side effects on children born from frozen eggs. Ongoing research aims to provide more comprehensive long-term data. If concerns exist, discussing them with a fertility specialist can provide personalized insights based on the latest research.
How Many Eggs Should a Woman Freeze?
Determining the exact number of eggs to freeze can be challenging as it depends on various factors, including ovarian reserve and age. An initial ovarian reserve assessment through an AMH test and ultrasound can help estimate the potential yield of eggs. Typically, freezing 15-20 eggs is recommended to increase the likelihood of a successful pregnancy, though this number may vary based on individual circumstances. Younger women generally have a higher success rate while those over 37-38 may require more cycles to achieve a comparable number of eggs.
A Society Fit for Children
The Importance of Child Welfare in a Civilized Society
“A nation’s children are its supremely important asset and the nation’s future lies in their proper development. An investment in Children is indeed an investment in the nation’s future. A healthy and educated child of today is the active and intelligent citizen of tomorrow. Bestow blessings on these little innocent lives bloomed on earth, who have brought the message of Joy from the heavenly garden”. - Rabindranath Tagore
To create a world suitable for children, a society must prioritize the care of its most vulnerable members—its children. In a truly civilized society, the well-being of children is fundamental as the health and development of children directly influence the prosperity and growth of the entire community. Every child is unique and represents an invaluable national asset.
However, this idealistic vision often feels deep when confronted with the harsh realities of neglect, abuse, and exploitation that children face daily. Poverty, illiteracy, and social structures leave children susceptible to harm from parents, relatives, employers, or strangers who often act in their self-interest without considering the children's need for healthy growth and development. These vulnerable children become easy targets for exploitation and mistreatment and they can be manipulated by anti-social elements. Recognizing these challenges, the Convention on the Rights of the Child was adopted in 1989 to provide special consideration to children living in exceptionally difficult conditions.
The Rise of Surrogacy and Associated Challenges
Recent advancements in medical science have made human reproduction possible through advanced technology, such as in-vitro fertilization (IVF). This has given rise to surrogacy where individuals or couples can engage a surrogate to carry a child for them. The embryos implanted in the surrogate can be created from the commissioning of parents' gametes or donated ones. Typically, a legal agreement is made between the commissioning parents and the surrogate by outlining the responsibilities and compensation, whether the surrogacy is selfless or commercial. The surrogate agrees to carry and deliver the baby to the commissioning parents, relinquishing any parental rights over the child.
Abandonment and Neglect in Surrogacy
A new form of abuse has emerged from the abandonment of children born to surrogates. Despite agreements, commissioning parents sometimes refuse to accept the child due to reasons like divorce, the child's disability, gender, appearance, or the birth of multiple children. This situation leaves the surrogate struggling with the child's care.
For instance, an Australian couple, David and Wendy Farnell, refused to accept their surrogate-born son Gammy, who had Down’s syndrome, while taking his healthy twin sister. The surrogate, Pattaram Chanbua was left to care for Gammy, who had severe health issues. Despite moral condemnation, there was no legal compulsion for the couple to take Gammy.
Similarly, another Australian couple rejected a twin born to an Indian surrogate because of its gender and they applied for Australian citizenship for only one child. This left the other child stranded with India taking responsibility for its welfare. The child faced potential trafficking risks due to the lack of official parents or citizenship.
In another case, a mix-up of gametes resulted in twins where one was Caucasian and the other was Indian. The Australian parents took the Caucasian child by leaving the fate of the Indian child uncertain. A British surrogate mother experienced a similar situation where the intending parents took the healthy twin and rejected the disabled one by referring to the child disapprovingly.
The Need for International Standards and Regulations
The lack of international standards and regulations for surrogacy poses significant child protection concerns. Without proper rules, screening or assessment of intending parents, children born through unregulated surrogacy arrangements are at risk of abuse or trafficking. It is imperative to establish comprehensive international guidelines to safeguard the rights and well-being of these children. By addressing these issues, society can take a crucial step towards ensuring that the welfare of children as envisioned in a civilized world is not just rhetoric but a reality.
Rights of Children Born through Assisted Reproductive Technology: An Indian Perspective
The Evolution of Child Rights in India
Children have the right to equal opportunities, dignity, care, protection and rehabilitation from society. This support should help integrate them into mainstream social life without facing prejudice for circumstances beyond their control. Instruments like the Convention on the Rights of the Child (CRC), the fundamental rights in Part III of the Indian Constitution, the Universal Declaration of Human Rights and the Directive Principles of State Policy collectively aim to improve the social, educational and cultural conditions of children by giving them opportunities similar to those available to other children. Every child inherently has the right to life and from birth the right to dignity.
The Indian Constitution is the foundation of the child rights movement in the country. It guarantees fundamental rights to children by enabling the creation of laws that provide them with special protection. Article 21 of the Constitution explicitly states that every child has the inherent right to life, which encompasses the right to live with dignity. Living with dignity means more than just physical existence; it includes the right of every child to develop fully as a human being.
Legal Protections for Children Under CRC
The CRC (Convention on Rights of Children) grants numerous rights to children without discrimination by applying equally to children born through assisted reproductive technology (ART). These children should not face discrimination based on the circumstances of their birth or the method of their conception. Recognizing children's rights emphasizes their value as individuals rather than mere objects of concern.
However, existing laws were primarily designed with naturally born children in mind. These laws are based on the premise of natural birth without the involvement of technology. As a result, children born through ART may not be adequately covered by these laws, leading to potential discrimination regarding their legitimacy, status, parenthood, and inheritance.
Addressing Discrimination Against Children Born Through ART
Children born through ART must be afforded the same rights as those born naturally to ensure they are not marginalized. The current legal framework must evolve to recognize and protect the unique circumstances of ART births, ensuring that these children receive equal treatment in all aspects of life. By doing so, society can uphold the principles of equality and dignity enshrined in the Constitution and international agreements. Further, ensuring that every child, regardless of their birth circumstances can thrive and develop to their fullest potential.
India’s Commitment to Protecting Children’s Rights are they really in a position with the CRC?
As a signatory to the Convention on the Rights of the Child (CRC), India is committed to safeguarding the rights of all children including those born through assisted reproductive technology (ART). To meet these obligations, all child-related legislation must align with CRC standards. This requires a strong connection between the principles outlined in the CRC and national laws. Developing a child-focused culture involves creating policies, practices, structures and laws that protect children and their rights comprehensively.
Legislative Efforts to Protect Children
India has implemented several laws to uphold the rights granted to children under the CRC. These include:
- The Juvenile Justice (Care and Protection of Children) Act, 2000 (JJ Act)
- The Child Labour (Prohibition and Regulation) Act, 1986
- Child Marriage Restraint Act, 1929
- Young Persons Harmful Publication Act, 1956
- The Prohibition of Child Marriage Act, 2006
- Commission for Protection of Child Rights Act, 2005
- The Children (Pledging of Labour) Act, 1953
- Protection of Children from Sexual Offences Act, 2012.
In 2003, the Government of India adopted the National Charter for Children which mandates that the State and community undertake all possible measures to ensure the protection, survival, life and liberty of all children.
National Commission for Protection of Child Rights
The National Commission for Protection of Child Rights is tasked with reviewing the safeguards provided by laws for child protection and recommending measures for their effective implementation. It studies international treaties and instruments, periodically reviews, existing policies and programs on child rights, and investigates violations of child rights.
Concept of Legitimacy in India
Traditional Views on Legitimacy
Indian courts have consistently held that a child born within marriage and lawfully affected is legitimate. Legitimacy is a status conferred by society, recognizing children born within legal marriages as legitimate. The term "illegitimate" refers to children not born within a lawful marriage. Although Section 16 of the Hindu Marriage Act, 1955 and Section 21 of the Divorce Act, 1869 offer some protection to children born out of void or voidable marriages these protections are limited. Consequently, innocent children suffer societal stigma and disadvantages due to circumstances beyond their control and in recognizing the legitimacy of the children then they are being labelled as illegitimate for their parents' actions.
Legitimacy and Assisted Reproductive Technology
ART can be utilized by married couples, unmarried couples or single individuals. The legitimacy of children born through ART to unmarried couples or single individuals depends on the governing personal laws. For example, under the Hindu Succession Act, 1956, a child born to a single woman is considered legitimate. In contrast, under Mahomedan law, a child born to a single unmarried woman is regarded as nullius filius (child of no one).
In India, personal laws such as the Hindu Succession Act, 1956, the Indian Succession Act, 1925, and Mahomedan Law determine the legitimacy of a child. These laws need to be revisited to ensure that children born through ART ( Assisted Reproductive Technology ) are not unfairly discriminated against and are given the same rights and recognition as other children.
Conclusion
The likelihood of achieving a live birth is comparable between vitrified and fresh eggs used in IVF treatments. The two pivotal factors influencing the success of using frozen eggs are the woman's age at the time of egg freezing and the quantity of eggs stored. As women age, particularly from their early thirties to late thirties and early forties, both the number and quality of eggs that develop in response to ovarian stimulation decline. The importance of the quantity and quality of eggs is highlighted by the fact that at each step—retrieval, freezing, fertilization, and embryo development—there is a risk of losing some eggs.
Not all retrieved eggs are suitable for freezing; some do not survive the freezing process and others may not fertilize or develop into healthy embryos. Furthermore, not all transferred embryos result in pregnancy, and some pregnancies may end in miscarriage. Current research indicates that vitrified oocytes yield better IVF outcomes than slow-frozen oocytes and may offer similar results to using fresh oocytes in certain patient groups. Cryopreserved oocytes can be particularly beneficial for patients facing infertility due to age or disease, those involved in oocyte donation programs, couples with difficulties producing semen on demand and patients with ethical or legal concerns about embryo cryopreservation. Additionally, egg freezing avoids some of the ethical issues associated with embryo freezing.
Disclaimer: This article is based on various facts and references taken from research blogs, Media resources, and studies. It doesn't attempt to hurt any sentiments and doesn’t discriminate among any ethnic community, caste, religion, gender, sex, or place of birth. The author and Reflections.live team are not liable for any sort of legal action against them. This article contains details based on treatments and surgeries, which some readers may find distressing. By reading this blog, readers give consent that the views in this article are opinions and readers might agree or disagree with the same for which they can’t sue the author or Reflections.live team or people associated with this blog directly or indirectly, for any sort of disagreements in case they have. Further Reflections.live team and the author have high regard and respect for all opinions.
. . .
References: