Something really scary is happening in hospitals everywhere. People are dying from bacterial infections that doctors used to treat easily with antibiotics. This is not some problem that might happen in the future. It is happening today, right now. The bacteria got smarter and evolved faster than scientists could make new medicines. We are running out of ways to fight them. But there is an unusual weapon that we overlooked for almost a hundred years. Bacteriophages are viruses that hunt down bacteria and destroy them with amazing accuracy.
When I first heard about phage therapy, I thought it sounded crazy. Using viruses to cure infections? It seemed like something from a science fiction movie. But as I learned more and read the research papers, I got really fascinated. These tiny predators have been perfecting their skills at killing bacteria for billions of years. They might be exactly what we need right now to fight antibiotic resistance.
The Molecular Machinery: How Phages Actually Kill Bacteria
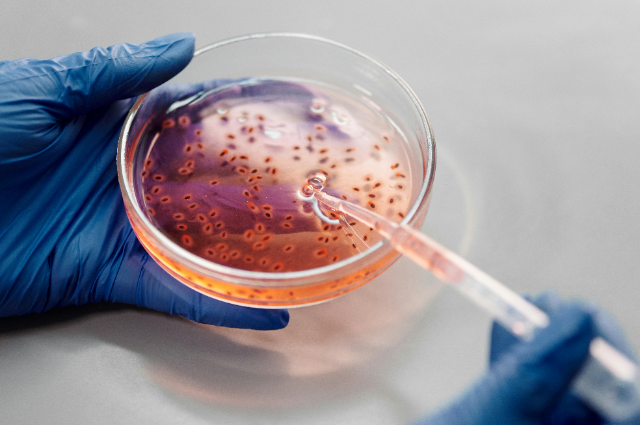
Let me explain what happens when a bacteriophage finds its target bacterium. This is not just a simple case of a virus meeting bacteria and bacteria dying. It is actually an intricate process that becomes absolutely fascinating once you understand how it works.
Picture a bacteriophage in your mind. It looks completely different from the viruses that give us colds or the flu. Most phages that doctors want to use for treatment look like something from a science fiction movie. They have a twenty-sided geometric head packed full of genetic material. This head sits on top of a tail structure with spider-like fibres sticking out from the bottom. That head contains tightly coiled DNA or RNA compressed to incredibly high densities.
The infection starts with recognition. Those tail fibres are not just for decoration. They work as highly specific molecular sensors. They scan the surface of bacteria looking for exact protein or sugar patterns, kind of like a key searching for the one lock it fits. This explains why phages are so selective about what they infect. A phage that attacks E. coli bacteria will not even recognise Staphylococcus aureus bacteria, and the other way around, too. Sometimes the pickiness goes even deeper. Certain phages only attack particular strains within one species.
Once the phage locates its target and attaches to the bacterial surface, something amazing happens. The tail works like a molecular syringe. The phage literally punches a hole through the bacterial cell wall and membrane using special enzymes that break down the protective layers. In some types of phages, the tail sheath contracts like a tiny muscle. This drives a hollow needle through the bacterial defences. The pressure inside that microscopic phage head is enormous, about 60 atmospheres. That is similar to the pressure you would find in a champagne bottle. When that seal breaks, the genetic material from the phage gets forcefully injected into the bacterial cell (Gordillo Altamirano & Barr, 2019).
Now here is where things get really interesting. Once the phage genome is inside, it completely hijacks the bacterial machinery. Think of it like a hostile takeover of a factory. The bacterial ribosomes normally make proteins that the bacterium needs to survive. Suddenly, they start producing phage proteins instead. The system that bacteria use to copy their DNA starts copying phage genes. Within just a few minutes, the entire bacterial cell is working for the phage.
The phage genome usually encodes somewhere between 40 and 200 different proteins. Each protein has a specific job to do. Some early proteins shut down the defences that bacteria have. Other proteins redirect the bacterial metabolism toward making phage components. As the infection continues, the cell starts putting together new phage particles. Heads get stuffed with DNA, tails get constructed, fibres get attached. It looks like a microscopic assembly line running at maximum speed.
This whole process takes about 20 to 40 minutes for most phages that doctors use for therapy. During that time, anywhere from 50 to 200 baby phages get assembled inside the doomed bacterium. Then comes the dramatic finale, which scientists call lysis. The phage makes enzymes with names like holins and endolysins. Holins create holes in the bacterial inner membrane. Endolysins break down the cell wall from the inside. The bacterial cell literally explodes and releases all those newly made phages into the surrounding environment. These new phages then continue the infection cycle.
What strikes me as elegant about this mechanism is that it stops itself naturally. If bacteria are present, phages multiply exponentially right at the infection site. But once all the bacteria that can be infected are dead, the phages have nothing left to attack. They just get cleared from the body through natural processes. You do not need to worry about stopping treatment at the right time or dealing with leftover medication. The treatment stops when the job is finished.
The Tom Patterson Case: When Medicine Got Desperate
The Tom Patterson story is not some obscure case that I dug up from old medical journals. It is probably the most well-documented and influential phage therapy case in modern Western medicine. The case was published in 2017 in the prestigious journal Antimicrobial Agents and Chemotherapy.
Tom and his wife Steffanie were on vacation in Egypt back in late 2015. Tom was a 68-year-old psychology professor who started feeling some pain in his abdomen. Within just a few days, he became critically ill. He had a pancreatic pseudocyst that got infected with a bacterium called Acinetobacter baumannii. This bacterium is on the World Health Organisation's priority list of antibiotic-resistant pathogens. Medical teams airlifted Tom back to UC San Diego, where doctors fought hard to save his life.
They tried absolutely everything they had available. They used colistin, which is one of our last resort antibiotics. They tried multiple carbapenems. They used different aminoglycosides. Nothing worked at all. Tom slipped into a septic coma while his organs started failing one by one. The bacteria had formed biofilms on drainage tubes placed in his abdomen. These biofilms created protected reservoirs that kept reseeding the infection over and over. His doctors ran out of options completely and told Steffanie to prepare herself for the worst outcome.
But Steffanie works as an infectious disease epidemiologist. She knew about phage therapy from her work studying epidemics in places with limited medical resources. In those settings, experimental treatments sometimes get tried out of sheer desperation. She started frantically sending emails to researchers all around the world, asking if anyone could help save her husband.
What happened next involved an unprecedented level of collaboration. Researchers at the Naval Medical Research Centre started screening their phage collections against Tom's bacterial isolate. Teams at Texas A&M did the same thing. They tested hundreds of different phages to find ones that could kill his specific strain of bacteria. This was not just about finding any phage that attacks Acinetobacter. It had to work against the exact bacteria making Tom sick.
They identified four different phages that showed real promise. Some of these phages came from sewage samples, because phages are really abundant in wastewater, where they constantly prey on bacteria. Other phages came from research collections that labs had been building for years. The team had to rapidly produce these phages in large quantities, purify them properly, and conduct basic safety testing. All of this happened while Tom was dying.
The FDA allowed the treatment under something called an emergency investigational new drug application. In March 2016, doctors started giving Tom the phages through his veins and through the abdominal drains. They also kept using antibiotics at the same time, creating a combination therapy approach (Tagliaferri et al., 2019).
The response was really dramatic. Within 48 hours after starting phage therapy, Tom's clinical condition began improving. He woke up from his coma. His fever went away. Blood tests showed his white blood cell count getting back to normal levels. Over the weeks that followed, the infection cleared up completely. Tom eventually recovered and is alive and well today, sharing his story with anyone who will listen.
What makes this case so incredibly valuable is not just that it worked. It is that everything was meticulously documented. The researchers published detailed protocols explaining exactly what they did. They described the phage selection process step by step. They monitored Tom's immune responses carefully. They tracked how both the bacteria and phages evolved during treatment. The case became a roadmap showing that personalised phage therapy was actually possible in a modern medical setting, even though it required extraordinary effort from many people.
Why Phages Succeed Against Biofilms When Antibiotics Fail
There is a particular problem in infectious diseases that does not get talked about enough. The problem is biofilms. I mentioned them when discussing Tom's case, but let me explain why they create such a nightmare for doctors and why phages might be uniquely suited to dealing with them.
Biofilms are bacterial communities that are encased in a matrix that the bacteria produce themselves. This matrix contains proteins, sugars, and even DNA. Think of biofilms as bacterial cities, complete with infrastructure. Individual bacteria floating around in blood or tissue are relatively vulnerable. Antibiotics can reach them, and immune cells can attack them. But bacteria living in biofilms have serious protection.
The biofilm matrix itself creates a physical barrier. Many antibiotics cannot penetrate this barrier very well. It is not completely impenetrable, but it dramatically reduces how much drug actually reaches bacteria deep inside the biofilm. Even worse than that, bacteria in biofilms often enter dormant states where they are not actively growing. Most antibiotics work by messing with bacterial growth processes like protein synthesis, cell wall construction, or DNA replication. If bacteria are not actively doing those things, the drugs simply do not work.
Here is where it gets really frustrating from a clinical perspective. Biofilms form on virtually every medical device that doctors implant in patients. Catheters get biofilms. Artificial joints get biofilms. Heart valves, pacemaker leads, and prosthetic blood vessels all get biofilms. Anywhere there is a foreign surface touching body fluids, biofilms can develop. Once these infections get established, they become incredibly difficult to clear using antibiotics alone. Often, the only real solution involves surgically removing the device. That is obviously not ideal when we are talking about someone's artificial hip or their heart valve.
Phages attack biofilms in a completely different way than antibiotics do. First, phages are really small. A typical phage might be about 100 nanometers, compared to a bacterium that could be 1000 to 2000 nanometers. This size difference really matters because phages can navigate through the biofilm matrix much more easily than larger molecules can.
But size is not the whole story here. Many phages produce enzymes that are specifically designed to break down biofilm components. Some make depolymerases that degrade the extracellular sugars holding the matrix together. Other phages make enzymes that break apart the protein scaffolding. Some even chew up the extracellular DNA that bacteria use as structural material in their biofilms (Gordillo Altamirano & Barr, 2019).
Once a phage gets inside the biofilm and infects a bacterium, something interesting happens. Remember how I described lysis, where the bacterial cell bursts open? When that happens deep inside a biofilm, it releases not just more phages but also all the enzymes those phages produce. Suddenly, you have these bacteria degrading enzymes getting released right in the heart of the biofilm structure. They start breaking it down from the inside out.
The other advantage is multiplication. Doctors might deliver a relatively modest initial dose of phages to start. But if the phages successfully infect bacteria in the biofilm, they will replicate right there at the infection site. The concentration of phages increases exactly where you need it most. Antibiotics do not do this at all. You give a dose, it distributes through the body, gets broken down and removed, and concentrations just keep declining over time.
The Evolutionary Arms Race: Why Resistance Isn't the End
Whenever I talk to people about phage therapy, someone always asks me this question. Won't bacteria just develop resistance to phages the same way they developed resistance to antibiotics? It is actually a really smart question to ask. The answer is yes, bacteria absolutely can develop resistance against phages. But here is why that fact is not necessarily a deal breaker for phage therapy.
Bacteria and phages have been locked in evolutionary combat for billions of years. It is genuinely the longest-running arms race in all of biological history. Bacteria evolve various defence mechanisms. They modify the surface receptors that phages use to attach. They develop restriction enzymes that cut up foreign DNA. They even use CRISPR systems, which originally evolved as a bacterial immune system specifically against phages. Phages, in turn, evolve counter-strategies to overcome every defence that bacteria develop.
This evolutionary dynamic is fundamentally different from our situation with antibiotics. Antibiotics are static chemical compounds that do not change. When bacteria evolve resistance to them, that is pretty much it. The drug stops working. We cannot easily modify the antibiotic molecule in response to bacterial evolution. With phages, we actually can.
If bacteria in a patient develop resistance to one particular phage, researchers can go out and isolate new phages from environmental sources. These new phages can overcome that resistance. Alternatively, researchers can use genetic engineering to modify the phage they already have. They might change the tail fibre proteins that recognise bacterial surfaces, for instance. The key point is that phages are living, evolving entities that can be adapted to meet new challenges.
There is another fascinating angle to consider here. When bacteria evolve resistance against phages, they often end up paying a fitness cost. For example, imagine a bacterium mutates the surface receptor that a phage uses to attach. That receptor probably had some normal biological function for the bacterium. Maybe it was an iron uptake channel, or maybe it transported sugars across the membrane. Losing that receptor or modifying it might make the bacterium less efficient at gathering nutrients. It might make the bacterium less virulent and less able to cause disease.
Some researchers are deliberately trying to exploit this trade-off. They use phages not necessarily to kill all the bacteria outright. Instead, they use phages to drive bacteria into evolutionary corners where the bacteria become less dangerous or more susceptible to antibiotics again. It is a subtle approach that uses evolution itself as a tool rather than just hitting bacteria with brute force (Tagliaferri et al., 2019).
The Practical Challenges Nobody Warned You About
I have painted a pretty optimistic picture so far in this article. But I need to be completely honest about the significant challenges that make phage therapy difficult to use widely in medicine. These are not just bureaucratic hurdles or red tape. They are real scientific and practical problems that need actual solutions.
First, there is the time issue that nobody talks about enough. When someone has a severe infection, doctors need to start treatment immediately, within hours. With antibiotics, you can literally grab a broad-spectrum drug off the shelf and begin treatment within minutes of diagnosis. With phages, you ideally need to identify exactly what bacteria are causing the infection first. Then you need to isolate phages that work against that specific bacterial strain. Then you test them to make absolutely sure they are effective. Then you have to grow enough phages for treatment. Then you purify them. Then you formulate them into a safe preparation that can be given to patients. Even with the very best protocols and experienced teams, this whole process takes days at a minimum.
Some researchers are working hard on what they call phage banks. These are basically libraries of well-characterised phages that are ready to use against common pathogens. The idea is that you would have cocktails prepared in advance that cover the most frequent bacterial strains causing specific types of infections. It represents a compromise between complete personalisation and practical usability. But it could make phage therapy much faster to deploy in emergencies.
Then there is the manufacturing challenge that pharmaceutical companies struggle with. These companies know exactly how to make chemical drugs at a massive scale with consistent quality every single time. Growing viruses is significantly trickier than synthesising chemicals. Phages can mutate during the production process. Bacterial debris from the growth process needs to be removed without damaging the phages themselves. Storage conditions really matter. Some phages remain stable at room temperature, while others absolutely need refrigeration. You need to ensure the preparation actually contains infective phages, not just dead phage particles that look perfectly fine under a microscope but do not work at all.
Quality control becomes its own massive headache. How exactly do you standardise a living product that might evolve? What metrics should be used to measure quality? With chemical drugs, you simply measure concentration and purity using analytical chemistry. With phages, you need to measure infectivity, meaning how well they actually kill bacteria in real conditions. That requires biological assays that are much more complex and time-consuming than simple chemical analyses.
The regulatory pathway is probably the single biggest obstacle preventing widespread adoption. The FDA and European Medicines Agency have established frameworks designed specifically for chemical drugs or biological products like monoclonal antibodies. Phages do not fit neatly into either category. They are alive. They evolve. They might need to be personalised for individual patients. None of this aligns well with traditional drug approval processes that fundamentally assume standardised, reproducible products that remain identical batch after batch.
Different countries are experimenting with different regulatory solutions. Belgium created something called a magistral preparation framework. Under this system, hospital pharmacies can prepare patient-specific phage treatments with appropriate oversight. It works similarly to how compounding pharmacies make customised medications for individual patients, but with more regulatory scrutiny. France has established emergency access programs. The United States allows compassionate use for individual patients facing life-threatening situations, but there is no clear pathway established yet for broader approval and routine clinical use.
Where I Think This Is All Heading
After spending a considerable amount of time researching this whole topic, I have developed some thoughts about what the realistic future of phage therapy might actually look like. I genuinely do not think phages will replace antibiotics entirely. That expectation is neither realistic nor even desirable. But I do think phages will eventually find their proper place in our medical toolkit.
The most immediate applications will probably focus on infections that are both serious and extremely difficult to treat using conventional methods. Chronic biofilm-associated infections on medical devices represent one clear target. Multidrug-resistant bacteria in critically ill patients represent another. Infections in immunocompromised people who cannot tolerate harsh antibiotic regimens also make sense. These are situations where the complexity and significant cost of phage therapy are justified by the severity of the underlying problem.
I imagine specialised phage therapy centres will eventually emerge in major medical centres. These would work similarly to how we currently have specialised transplant centres or dedicated cancer treatment facilities. These centres would have the necessary expertise, the required infrastructure, and comprehensive phage collections needed to rapidly characterise bacterial infections and match them with appropriate therapeutic phages. Primary care doctors would not need to become phage experts themselves. They would simply refer their most complex cases to these specialised centres.
Advancing technology will definitely help move things forward. Rapid diagnostic tools using whole genome sequencing or mass spectrometry could potentially identify bacterial strains in just a few hours rather than taking days. Artificial intelligence systems could potentially predict which phages are most likely to work against specific bacterial genotypes. This would eliminate the need to physically test every possible combination. These kinds of advances could make phage therapy much faster and significantly more accessible to patients who need it.
I feel particularly excited about combination approaches that use multiple treatment methods together. Using phages together with antibiotics is not just additive, where you add the two effects together. There is actually evidence of real synergy where the combination works considerably better than you would predict from simply adding the individual effects. Maybe antibiotics weaken bacterial defences in ways that make bacteria more susceptible to phage attack. Maybe phages break up biofilms in ways that allow antibiotics to penetrate better. We definitely need more research to fully understand these interactions, but the preliminary results look really promising.
Preventive applications also intrigue me quite a bit. Imagine coating urinary catheters with appropriate phages before insertion into patients. This could prevent biofilm formation from happening in the first place. Or picture using phages in specialised wound dressings designed for burn patients who face extremely high risks of developing resistant infections. These prophylactic uses might actually be easier to regulate and implement than therapeutic uses because the regulatory requirements for prevention are sometimes less stringent than requirements for treatment.
Conclusion
Look, I am not going to sit here and pretend that phage therapy is ready to save the entire world tomorrow morning. We genuinely have real work ahead of us. Clinical trials need to be completed properly. Regulations need to be navigated carefully. Infrastructure needs to be built from scratch in many places. Doctors need to be trained on something completely new. Some of the enthusiasm I see in popular articles really oversimplifies the significant challenges we face.
But here is what keeps me personally interested and engaged with this topic. We genuinely need alternatives to antibiotics, and we need them very soon. The antibiotic resistance crisis is not some hypothetical problem that might happen someday. It is here right now, today. I have read far too many case reports and research papers about patients with completely untreatable infections to think we can just keep doing what we have always been doing. That approach is clearly not working anymore.
Phages offer something genuinely different from anything else we have tried. This is not just another chemical antibiotic that bacteria will inevitably develop resistance against within a few years. This is a dynamic, evolutionary approach that can continuously adapt as bacteria themselves adapt. The underlying mechanism is genuinely elegant. The specificity provides real value in preserving beneficial microbiomes. The preliminary evidence, while admittedly still limited, looks genuinely encouraging.
The Tom Patterson case demonstrated pretty clearly that personalised phage therapy is actually possible within a modern medical system. Yes, it required truly extraordinary circumstances and massive collaborative effort. Now we need to figure out how to make it less extraordinary and more routine. We need to streamline the entire process. We need to reduce both the time required and the costs involved. We need to develop clear quality standards that everyone can follow. We need to train clinicians properly. We need to integrate phage therapy smoothly into existing treatment protocols and clinical workflows.
I genuinely think we will eventually get there. It will not happen quickly. It will not happen easily. But I believe it will happen eventually. And when we finally do get there, we will have a genuinely powerful tool for fighting bacterial infections that we desperately need right now. That realistic possibility makes all the current challenges absolutely worth working through, despite how difficult and frustrating the process sometimes feels.
References
