
INTRODUCTION
We may know the most common negative impacts of war which includes loss of human lives, economic losses due to the destruction of capital as well as disruption of trade, the spread of diseases, displacement of people, and destruction of the environment. But not many talk about the impact of the War on Mental Health. Let’s see it in detail about this issue.
WHAT IS WAR?
War is generally defined as a violent conflict between states or nations.

REASON FOR WAR
Nations go to war for a variety of reasons. It has been argued that a nation will go to war if the benefits of war are deemed to outweigh the disadvantages and if there is a sense that there is not another mutually agreeable solution. More specifically, some have argued that wars are fought primarily for economic, religious, and political reasons. Others have claimed that most wars today are fought for ideological reasons.
'War does not determine who is Right - Only who is Left”
IMPACT OF WAR ON MENTAL HEALTH
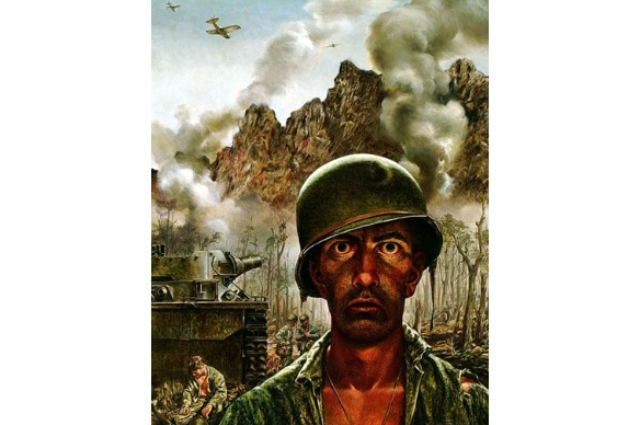
A traumatic event is a shocking, scary, or dangerous experience that affects you emotionally. During the war, people can be exposed to many different traumatic events. That raises the chances of developing mental health problems-like post-traumatic stress disorder (PTSD), anxiety, and depression-and poorer life outcomes as adults.
In some violent armed conflicts, children may be separated from their families and communities by armed groups. These “child soldiers” can witness or participate in killings and experience other traumatic events. In addition to the psychological trauma and physical injuries, many former child soldiers face rejection from family and community after the war.
Wars have had an important part in psychiatric history in a number of ways. It was the psychological impact of the world wars in the form of shell shock that supported the effectiveness of psychological interventions during the first half of the 20th century. It was the recognition of a proportion of the population not suitable for army recruitment during the Second World War that spurred the setting up of the National Institute of Mental Health in USA. The differences in the presentation of the psychological symptoms among the officers and the soldiers opened up new ways of understanding the psychiatric reactions to stress.
Though there have not been any world wars since the Second World War, there have been wars and conflicts throughout the last 60 years. For example, in the 22 countries of the Eastern Mediterranean region of the World Health Organization (WHO), over 80% of the population either is in a conflict situation or has experienced such a situation in the last quarter of a century.
War has a catastrophic effect on the health and well-being of nations. Studies have shown that conflict situations cause more mortality and disability than any major disease. War destroys communities and families and often disrupts the development of the social and economic fabric of nations. The effects of war include long-term physical and psychological harm to children and adults, as well as reduction in material and human capital. Death as a result of wars is simply the "tip of the iceberg". Other consequences, besides death, are not well documented. They include endemic poverty, malnutrition, disability, economic/ social decline and psychosocial illness, to mention only a few. Only through a greater understanding of conflicts and the myriad of mental health problems that arise from them, coherent and effective strategies for dealing with such problems can be developed.
The importance that the WHO attributes to dealing with the psychological traumas of war was highlighted by the resolution of the World Health Assembly in May 2005, which urged member states "to strengthen action to protect children from and in armed conflict" and the resolution of the WHO Executive Board in January 2005, which urged "support for implementation of programmes to repair the psychological damage of war, conflict and natural disasters”.
The WHO estimated that, in the situations of armed conflicts throughout the world, "10% of the people who experience traumatic events will have serious mental health problems and another 10% will develop behavior that will hinder their ability to function effectively. The most common conditions are depression, anxiety and psychosomatic problems such as insomnia, or back and stomach aches".
MENTAL HEALTH IN WAR AFFECTED COUNTRIES
Afghanistan:
More than two decades of conflict have led to widespread human suffering and population displacement in Afghanistan. Two studies from this country are significant in terms of both their scope and their findings.
The first study used a national multistage, cluster, population based survey including 799 adult household members aged 15 years and above. Sixty-two percent of respondents reported experiencing at least four trauma events during the previous ten years. Symptoms of depression were found in 67.7% of respondents, symptoms of anxiety in 72.2%, and post-traumatic stress disorder (PTSD) in 42%. The disabled and women had a poorer mental health status, and there was a significant relationship between the mental health status and traumatic events. Coping strategies included religious and spiritual practices.
The second study, using a cross-sectional multicluster sample, was conducted in the Nangarhar province of Afghanistan, to estimate the prevalence of psychiatric symptoms, identify resources used for emotional support and risk factors, and assess the present coverage of basic needs. About 1011 respondents aged 15 years and above formed the sample. Nearly half of the population had experienced traumatic events. Symptoms of depression were observed in 38.5% of respondents, symptoms of anxiety in 51.8% and PTSD in 20.4%. High rates of symptoms were associated with higher numbers of traumatic events experienced. Women had higher rates than men. The main sources of emotional support were religion and family.
The Balkans:
The conflict in the Balkans is probably one of the most widely studied in recent years. Mental health of survivors of both sides was examined.
An initial study among Bosnian refugees demonstrated an association between psychiatric disorders (depression and PTSD) and disability. A three year follow-up study on the same group concluded that former Bosnian refugees who remained living in the region continued to exhibit psychiatric disorders and disability after initial assessment.
A cross-sectional cluster sample survey among Kosovar Albanians aged 15 years or older found that 17.1% (95% CI 13.2%-21.0%) reported symptoms of PTSD. There was a significant linear decrease in mental health status and social functioning with increasing amount of traumatic events in those aged 65 years or older, and with previous psychiatric illnesses or chronic health conditions. Internally displaced people were at increased risk of psychiatric morbidity. Men (89%) and women (90%) expressed strong feelings of hatred towards the Serbs, with 44% of men and 33% of women stating that they would act on these feelings.
In a study of the mental health and nutritional status among the Serbian ethnic minority in Kosovo, the General Health Questionnaire (GHQ)-28 scores in the subcategories of social dysfunction and severe depression were high, with women and those living alone or in small family units being more prone to psychiatric morbidity. In a community sample of 2,796 children aged between 9 and 14 years, high levels of post-traumatic symptoms and grief symptoms were reported. This was related to the amount and type of exposure. Girls reported more distress than boys.
Cambodia:
Cambodia has had a long history of violence, highlighted by the civil war in the 1960s, culminating with the "Khmer Rouge" rule that destroyed the social fabric of the society. Studies have found that refugees had high levels of psychiatric symptomatology after 10 years.
Chechnya:
The human rights abuses in the Chechen population have been well documented . A report on a small number of Chechen asylum seekers in the UK adds to the evidence on the abuses and related psychological fallouts. Psychosocial issues were explored in a survey conducted in settlements housing displaced people. Two thirds of respondents agreed with the statement that the conflict has triggered mental disturbance or feelings of being upset. Nearly all respondents indicated that they had family members having difficulty in coping with their disturbance or upset feelings. Coping strategies used were praying, talking, keeping busy, and seeking the support of family members.
Iraq:
Iraq has been at war at numerous times in history: a series of coups in the 1960s, the Iran-Iraq war (1980-1988), the anti-Kurdish Al-Anfal campaign within the country (1986-1989), the Iraqi invasion of Kuwait resulting in the Gulf war (1991), and the conflict starting in 2003. The UN-imposed economic sanctions following the Gulf war have had a profound impact on the health of Iraqis. The human rights abuses have also been recorded.
There are few studies on the impact of these conflicts on mental health. A study on 45 Kurdish families in two camps reported that PTSD was present in 87% of children and 60% of their caregivers. A study on 84 Iraqi male refugees found that poor social support was a stronger predictor of depressive morbidity than trauma factors. During the last three years of occupation by foreign forces, there have been many news reports about the mental health of the population, but no systematic study.
Israel:
Israel has been in a situation of conflict for over four decades. A large number of systematic studies have been undertaken in different population groups. A recent study found that 76.7% of subjects exposed to war-related trauma had at least one traumatic stress-related symptom, while 9.4% met the criteria for acute stress disorder. The most common coping mechanisms were active information search about loved ones and social support. Another study reported that, twenty years after the war with Lebanon, an initial combat stress reaction, PTSD-related chronic diseases and physical symptoms were associated with a greater engagement in risk behaviours.
Lebanon:
Lebanon has been ravaged by a civil war (1975-1990) and by an Israeli invasion in 1978 and 1982. The mental health impact of these conflicts has been studied extensively.
A random sample of 658 people aged between 18 and 65 years was randomly selected from four Lebanese communities exposed to war. The lifetime prevalence of DSM-III-R major depression varied across the communities from 16.3% to 41.9%. Exposure to war and a prior history of major depression were the main predictors for current depression.
Palestine:
During the last decade a large number of studies have reported high levels of psychosocial problems among children and adolescents, women, refugees and prisoners in Palestine.
In a series of studies during the last 10 years from the Gaza Community Mental Health Centre, the most prevalent types of trauma exposure for children were witnessing funerals (95%), witness to shooting (83%), seeing injured or dead strangers (67%) and family member injured or killed (62%). Among children living in the area of bombardments, 54% suffered from severe, 33.5% from moderate and 11% from mild or doubtful levels of PTSD. Girls were more vulnerable.
Rwanda:
The physical and mental health problems of the survivors of the genocide in Rwanda have been well documented. There have been reports on the state of health among the large numbers of refugees (500,000-800,000 in five days) who fled to Goma, Zaire following the capture of the capital Kigali, but none of them has considered the mental health dimension.
Sri Lanka:
The conflict between the majority Sinhala and minority Tamil population in Sri Lanka has been ongoing for nearly 30 years. One of the first studies that looked into the psychological effects of the conflict on the civilian population was an epidemiological survey , which reported that only 6% of the study population had not experienced any war stresses. Psychosocial sequelae were seen in 64% of the population, including somatization (41%), PTSD (27%), anxiety disorder (26%), major depression (25%), alcohol and drug misuse (15%), and functional disability (18%). The breakdown of the Tamil society led to women taking on more responsibilities, which in turn made them more vulnerable to stress. Children and adolescents had higher mental health morbidity.
Somalia:
A study carried out in ex-combatants in Somalia found high psychiatric morbidity and use of khat. A UNICEF study found evidence of psychological effects of the prolonged conflict situation in a high proportion of a sample of 10,000 children. There is near total disruption of the mental health services in the country.
Uganda:
Sudanese refugees fled into northern Uganda in two major waves in 1988 and 1994. Symptoms of PTSD and depression were found to be highly prevalent among Sudanese children living in the refugee camps. Refugees had higher rates of individual psychopathology than the general population, and it was observed that the cumulative stress grew as the years in exile progressed. The consequences of long-term exile were still present 5-15 years later, with an increase in the rates of suicide and alcohol use.
RISK FACTORS FOR CHILDREN & WOMEN:

Post‐traumatic stress disorder (PTSD) and depression are the most common mental health disorders in the aftermath of war – for both adults and children. Women have an increased vulnerability to the psychological consequences of war. There is evidence of a high correlation between mothers' and children's distress in a war situation. It is now known that maternal depression in the prenatal and postnatal period predicts poorer growth in a community-based sample of infants. Social support and traditional birth attendants have a major role in promoting maternal psychosocial well being in war-affected regions. The association between gender- based violence and common mental disorders is well known. Despite their vulnerability, women's resilience under stress and its role in sustaining their families have been recognized.
There is consistent evidence of higher rates of trauma-related psychological problems in children. The most impressive reports are those from Palestine. Of the different age groups, the most vulnerable are the adolescents.
PTSD can occur in children after even a single traumatic event, but repeated or prolonged trauma increases the risk. The symptoms of PTSD vary; sufferers may show intense fear, helplessness, anger, sadness, horror or denial. They can also develop physical symptoms including headaches and stomach aches; show more sudden and extreme emotional reactions; or have problems falling or staying asleep. Children who experience repeated trauma may develop a kind of emotional numbing to deaden or block the pain and trauma. This is called dissociation.
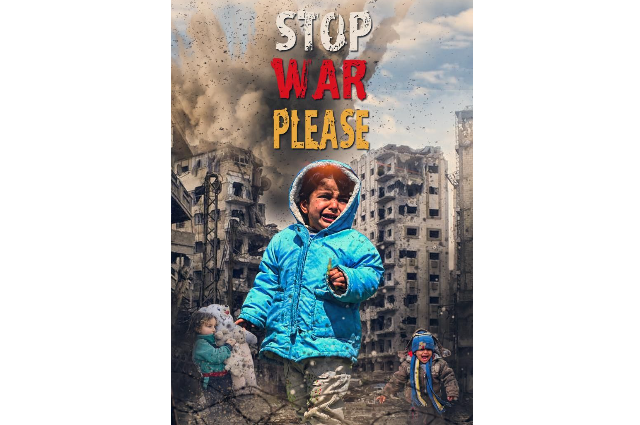
IMPACT ON UKRAINIAN CHILDREN

For many Ukrainian children, leaving their homes will also mean leaving their country. Displaced children, especially refugees, are more vulnerable to experiencing psychological issues. They also encounter additional risk factors and could be exposed to different forms of exploitation.
Studies have shown that children are particularly sensitive to an accumulation of stressors; in fact, there is considerable evidence for a dose‐response relation between the number of stressors experienced by children and their mental health outcomes. For child refugees, the accumulation of stress generally comes from three main contributors:
- In their native countries, many may have witnessed or experienced violence, torture and the loss of family and friends.
- The journey to a country of refuge can also be a time of further stress. Refugee children may experience separation from their parents, either by accident or as a strategy to ensure their safety.
- The final stage of finding respite in another country can be a time of additional difficulty as many have to prove their asylum claims and also try to integrate into a new society. This period is being increasingly referred to as a period of “secondary trauma” to highlight the problems encountered. On arriving, a refugee child will need to settle into a new school and find a peer group. Children might have to prematurely assume adult roles, for example, as a vital language link with the outside world.
Refugee children suffer both from the effects of coming from a war zone and of adjusting to an unfamiliar culture. These stressors also affect their families which in turn has an adverse effect on them. And the longer wars go on, the worse it is for children.
It is crucial that children are quickly integrated into the schools and healthcare systems of the countries they have taken refuge in. They will need emotional and psychological support from cross-cultural teams who can work in an extended outreach manner with children at schools and families at home. There is a need for a variety of different treatments, including individual, family, group and school-based interventions. Schools are uniquely placed to play a vital part in their integration by becoming an anchor, not only for educational but also for social and emotional development, and as an essential link between children, their parents and the local community.
CONCLUSION
It is time for health professionals to define war as a serious global public mental health problem. This issue needs to be addressed by WHO & UN-related bodies. Populations in war and conflict situations should receive mental health care as part of the total relief, rehabilitation, and reconstruction processes.
''Why use Weapons when we have Words to settle the Conflict”.
. . .
REFERENCES:
