
Photo by Mufid Majnun on Unsplash
Introduction:
Cervical cancer is a global health concern, with India recently taking a significant stride by introducing an indigenous HPV vaccine to combat this disease. In 2020, there were an estimated 604,000 new cases and 342,000 deaths globally, with the highest incidence and mortality rates found in low- and middle-income countries. India, in particular, grapples with cervical cancer, contributing to 6–29% of all cancers in women and ranking as the second leading cause of cancer deaths among women in the country. Human Papillomavirus (HPV) is a common sexually transmitted infection, responsible for cervical cancer development when persistent high-risk strains, such as HPV 16 and 18, are present. Lack of access to national HPV vaccination, cervical screening, and treatment services, along with social and economic factors, contribute to the inequities in cervical cancer incidence and mortality rates.
India's Serum Institute has developed "Cervavac," the country's first indigenous quadrivalent HPV vaccine effective against strains 6, 11, 16, and 18. A study in The Lancet Oncology demonstrated its comparable immune response to existing vaccines. Notably, Cervavac targets both girls and boys aged 9–26, a crucial inclusion for comprehensive preventive measures. "Cervavac" is set to be included in India's national program, aiming to address the financial barrier to vaccination. The Serum Institute plans to offer the vaccine at subsidised rates (Rs 200-400/-) for government programs and Rs 1400-1600/- per dose for private practitioners. This affordability is crucial, considering the high cost of existing vaccines like Gardasil (Rs 3500/-).
There is a need to raise awareness about the HPV infection and substantial percentage of cancers that are caused by this. Integration of cancer education and vaccination into every parent/caregivers into the family agenda should be advocated and a strategy for long term follow up of vaccinated girls should be built. Parents/caregivers of children must be educated regarding HPV vaccination before offering this chemoprophylaxis against cervical cancer. So let's try to understand,
WHAT IS CERVICAL CANCER?
We will understand the basic meaning first, by breaking the word cervical cancer. The cervix is the lower, narrow end of the uterus (womb). The cervix connects the uterus to the vagina (birth canal). Cancer is a disease in which cells in the body grow out of control. Cancer is always named for the part of the body where it starts, even if it spreads to other body parts later.
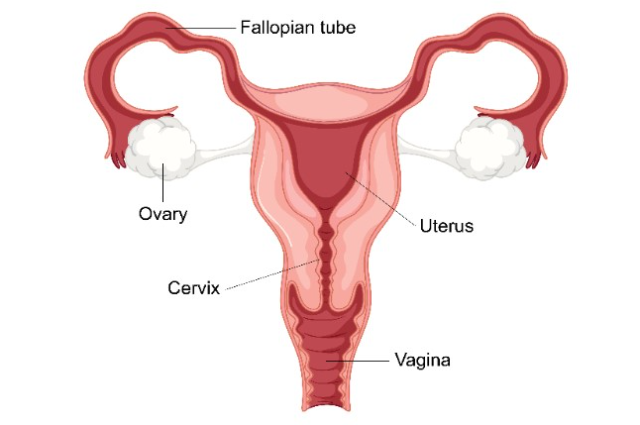
(Female Reproductive System) Image Credit: pregnancybirthbaby
When cancer starts in the cervix, it is called cervical cancer. Cervical cancer usually develops slowly over time. Before cancer appears in the cervix, the cells of the cervix go through changes known as dysplasia, in which abnormal cells begin to appear in the cervical tissue. Over time, if not destroyed or removed, the abnormal cells may become cancer cells and start to grow and spread more deeply into the cervix and to surrounding areas.
Cervical cancers are named after the type of cell where the cancer started. Two main types are squamous cell carcinoma and adenocarcinoma, with symptoms often appearing in advanced stages. Early detection through screening and vaccination is critical for effective treatment.
Symptoms :
It's really important to know the symptoms for early detection and prevention. Early on, cervical cancer usually doesn’t have symptoms, making it hard to detect. Symptoms usually begin after the cancer has spread. When symptoms of early-stage cervical cancer do occur, they may include,
- Vaginal bleeding after sex.
- Vaginal bleeding after menopause.
- Vaginal bleeding between periods or periods that are heavier or longer than normal.
- Vaginal discharge that is watery and has a strong odour or that contains blood.
- Pelvic pain or pain during sex.
Symptoms of advanced cervical cancer (cancer has spread beyond the cervix to other parts of the body) may include the symptoms of early-stage cervical cancer and;
- Difficult or painful bowel movements or bleeding from the rectum when having a bowel movement.
- Difficult or painful urination or blood in the urine.
- Swelling of the legs.
- Pain in the abdomen.
- Feeling tired.
These symptoms may be caused by many conditions other than cervical cancer. The only way to know is to see a health professional. If it is cervical cancer, ignoring symptoms can delay treatment and make it less effective.
Causes, Risk Factors, and Prevention:
Persistent infection with high-risk HPV types, especially 16 and 18, is the primary cause of cervical cancer. Nearly all people who are sexually active will become infected with HPV at some point in their lives. Most HPV infections go away on their own within a year or two as the immune system controls the infection. These short-term infections do not cause cancer. When a high-risk HPV infection lasts for years, it can lead to changes in the cervical cells, resulting in a precancerous lesion. If the precancerous lesion is not found and removed, it may eventually develop into cervical cancer. People who become sexually active at a young age, especially before age 18, or have multiple sexual partners are more likely to become infected with a high-risk type of HPV.
Risk factors include weakened immune systems, smoking, reproductive factors, obesity, and exposure to diethylstilbestrol (DES). DES exposure is a rare cause of cervical cancer Being exposed to a drug called diethylstilbestrol (DES) in the womb is an independent risk factor for a type of cervical cancer called clear cell adenocarcinoma.
Cervical cancer constitutes a significant health burden in India, causing approximately 1.23 lakh new cases and 77,000 deaths annually. The lack of effective screening and timely treatment contributes to India's disproportionate share of global cervical cancer deaths (25%).
- Cervical cancer is preventable.
Cervical cancer is highly preventable and highly curable if caught early. Nearly all cervical cancers could be prevented by HPV vaccination, routine cervical cancer screening, and appropriate follow-up treatment when needed.
Prevention Strategies:
To eliminate cervical cancer globally, affordable and accessible vaccines are essential. The availability of Serum's HPV vaccine, Cervavac, is seen as pivotal in enhancing global coverage for both girls and boys. The strategy emphasis vaccination for adolescent girls and cervical cancer screening for adult women using HPV tests as crucial preventive tools. Efforts must be made to raise awareness about HPV infections, the substantial link to cervical cancer, and the importance of vaccination and regular screening. Integrating cancer education into family agendas and establishing long-term follow-up strategies for vaccinated individuals can further strengthen preventive measures. Screening for cervical cancer, particularly through HPV and cytology tests, is crucial for early detection. HPV vaccination is a safe and effective preventive measure. Timely vaccination before sexual activity offers the most protection. Condoms, which prevent some sexually transmitted diseases, can decrease the risk of HPV transmission. However, they do not completely prevent it. Therefore, exposure to HPV is still possible in areas that are not covered by the condom.
The Centers for Disease Control and Prevention (CDC) recommends routine HPV vaccination for girls and boys at age 11 or 12, and the vaccine can be given starting at age 9. For young people who weren’t vaccinated within the age recommendations, HPV vaccination is recommended up to age 26. Some adults between the ages of 27 and 45 who are not already vaccinated may decide to get the HPV vaccine after talking with their doctor about their risk of new HPV infections.
The HPV vaccine is given as a series of two or three doses, depending on age. CDC recommends that children who start the vaccine series before age 15 receive two doses. For people who receive the first dose on or after their 15th birthday, and for people with certain immunocompromising conditions, CDC recommends getting three doses. Because HPV vaccination doesn’t protect against all HPV types that can cause cervical cancer, getting screened at regular intervals is still important. Two widely used screening tests are HPV tests and cytology tests (also known as Pap test or Pap smear). These tests can find high-risk HPV infections and abnormal cell changes and precancers that can be treated before they turn into cancer. So it is important for people with a cervix to have regular screening tests starting in their 20s.
Conclusion:
India's stride in developing and implementing the indigenous HPV vaccine, Cervavac, marks a significant step towards eliminating cervical cancer. With affordability, inclusion of both genders, and a comprehensive preventive strategy, the nation is poised to make a substantial impact in the global fight against cervical cancer. Raising awareness, integrating education into family agendas, and addressing barriers to access are crucial for the success of these preventive measures. The convergence of vaccination, screening, and treatment holds the key to a future where cervical cancer is highly preventable and curable when detected early.
