"As Polycystic Ovary Syndrome (PCOS) silently sweeps across the globe, affecting one in five women of reproductive age, it has become clear that this condition is more than just a reproductive health issue—it's a complex, multi-system disorder with profound implications for women's physical and mental well-being."
Polycystic ovary syndrome (PCOS) has emerged as one of the most prevalent hormonal disorders affecting women worldwide, with diagnosis rates climbing at an alarming rate. Despite its increasing prevalence, many individuals remain unaware of the serious long-term consequences associated with this condition. This article delves into the factors contributing to the surge in PCOS cases and the profound impact it has on women's lives. Beyond the common symptoms such as irregular periods and excessive hair growth, PCOS carries far-reaching implications that affect everything from cardiovascular health to mental well-being, highlighting the urgent need for awareness and understanding.
The Growing Prevalence of PCOS: A Modern Health Challenge
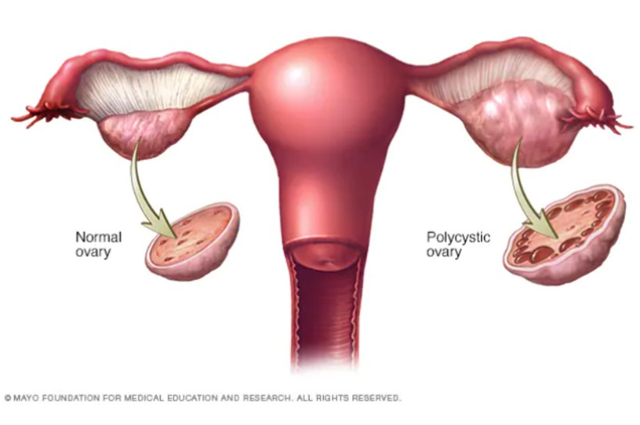
Polycystic ovary syndrome (PCOS) has emerged as one of the most prevalent hormonal disorders affecting women worldwide. Studies indicate a stark rise in PCOS diagnoses globally, with reports suggesting that nearly 20% of women of reproductive age may be affected. This alarming statistic highlights the scale of this health challenge, which has become increasingly prevalent in recent years.
While genetics play a significant role in the development of PCOS, with up to 70% of cases having a genetic component, the rapid increase in diagnosis rates points to the influence of lifestyle shifts and environmental factors in the modern world. The combination of genetic predisposition and environmental triggers has intensified the situation, leading to a surge in PCOS cases globally.
Lifestyle Factors
The modern lifestyle, characterized by urbanization, sedentary behaviors, and unhealthy dietary habits, has contributed to the rise in PCOS prevalence. The shift towards processed foods and a lack of physical activity has led to a significant increase in obesity rates, which is a major risk factor for PCOS.
Studies have found that the incidence of PCOS is 2-3 times higher among obese women compared to their non-obese counterparts. Excess weight can exacerbate insulin resistance, a hallmark of PCOS, leading to further hormonal imbalances and the development of associated health issues.
In addition to obesity, rising stress levels in the modern world have also been linked to the development and progression of PCOS. Chronic stress can disrupt the hypothalamic-pituitary-adrenal (HPA) axis, which plays a crucial role in regulating hormones, potentially contributing to the hormonal imbalances seen in PCOS.
Environmental Toxins
Exposure to endocrine-disrupting chemicals (EDCs) found in everyday products, such as plastics and cosmetics, is believed to be another contributing factor to the surge in PCOS cases. These chemicals can mimic or block natural hormones, interfering with the delicate hormonal interplay and potentially leading to hormonal imbalances.
EDCs can be found in a wide range of consumer products, including plastic containers, personal care items, and even in the food supply through pesticide residues. Prolonged exposure to these chemicals can disrupt the endocrine system, which is responsible for producing, secreting, and regulating hormones in the body.
The impact of EDCs on PCOS is an area of ongoing research, but studies suggest that these chemicals may contribute to the development and progression of the condition by altering hormonal balance and promoting insulin resistance.
Better Awareness & Diagnosis
Despite the rising prevalence of PCOS, many women remain undiagnosed or misdiagnosed. In the past, lack of awareness and understanding of the condition led to many women living with PCOS without proper diagnosis or treatment. However, even today, a significant proportion of patients with PCOS remain undiagnosed after visiting multiple medical institutions.
Estimates suggest that 68-75% of women with PCOS are undiagnosed, highlighting the need for better awareness and improved diagnostic criteria. With increased awareness and education, more women are seeking diagnosis and treatment for PCOS. Early diagnosis is crucial for managing the condition and preventing or delaying the onset of associated health complications.
The Burden of PCOS
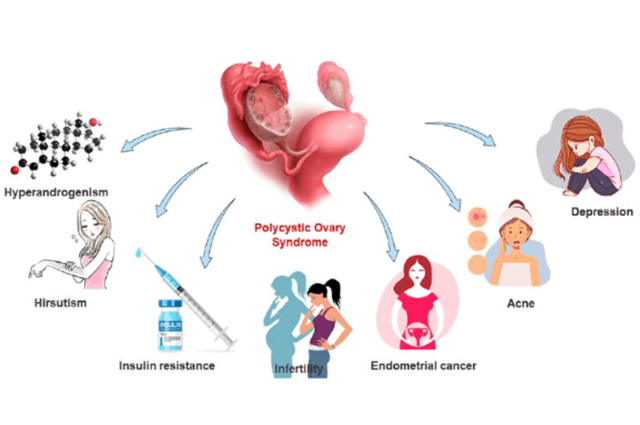
PCOS is not just a reproductive health issue; it carries significant long-term consequences that can impact various aspects of a woman's life. Women with PCOS are at higher risk of developing type 2 diabetes, cardiovascular disease, infertility, and mental health disorders like depression and anxiety.
The global burden of PCOS is substantial, with 1.55 million incident cases and 0.43 million associated disability-adjusted life years (DALYs) in 2017. This highlights the significant impact PCOS has on women's health and well-being, as well as the economic burden it places on healthcare systems worldwide.
Type 2 diabetes is a common complication of PCOS, with up to 50% of women with PCOS developing the condition by the age of 40. Cardiovascular disease is another major concern, as PCOS is associated with an increased risk of hypertension, dyslipidemia, and metabolic syndrome.
Infertility is also a significant issue for women with PCOS, with up to 74% experiencing difficulty conceiving. PCOS is one of the leading causes of female infertility, and many women with the condition require medical intervention to achieve pregnancy.
Mental health disorders, such as depression and anxiety, are also more prevalent among women with PCOS. The combination of physical symptoms, hormonal imbalances, and the challenges of managing a chronic condition can take a toll on mental well-being.
Understanding the Causes
Polycystic ovary syndrome (PCOS) is a complex endocrine disorder that affects a significant number of women globally. Understanding the causes of PCOS involves examining the interplay of hormonal imbalances, genetic predisposition, insulin resistance, and lifestyle factors.
Hormonal Chaos
PCOS is primarily characterized by hormonal chaos, particularly elevated levels of androgens, which are often referred to as male hormones despite being present in both genders. These elevated androgen levels can lead to a range of symptoms, including:
- Acne: Increased testosterone levels can stimulate oil production in the skin, leading to acne breakouts.
- Excessive Hair Growth (Hirsutism): Higher androgen levels can cause unwanted hair growth on the face, chest, and back, which can be distressing for many women.
- Irregular Menstrual Cycles: Hormonal imbalances can disrupt the normal ovulation process, leading to irregular or missed periods.
The hormonal imbalance in PCOS is not limited to androgens; it also involves other hormones such as luteinizing hormone (LH) and sex hormone-binding globulin (SHBG). Women with PCOS often have elevated LH levels and reduced SHBG, which can exacerbate the effects of excess testosterone.
Insulin Resistance
A significant proportion of women with PCOS struggle with insulin resistance, a condition where the body’s cells do not respond effectively to insulin, a hormone that regulates blood sugar levels. Insulin resistance is a key feature in 70-95% of women with obese PCOS and 30-75% of those with lean PCOS. This condition leads to several complications:
- Weight Gain: Insulin resistance often results in increased fat storage, making it challenging for women to maintain a healthy weight. Excess weight can further exacerbate insulin resistance, creating a vicious cycle.
- Increased Risk of Diabetes: The inability to effectively utilize insulin can elevate blood sugar levels, increasing the risk of developing type 2 diabetes. Women with PCOS are at a significantly higher risk of developing this condition due to the underlying insulin resistance.
- Hormonal Imbalances: High insulin levels can stimulate the ovaries to produce more testosterone, worsening the symptoms of PCOS and leading to further reproductive issues.
Genetic Predisposition
Genetics also play a crucial role in the development of PCOS. Women with a family history of the condition are more likely to develop it themselves, suggesting a hereditary component. While specific genes associated with PCOS have not yet been definitively identified, studies indicate that certain genetic factors may predispose individuals to hormonal imbalances and insulin resistance.
Research has shown that the heritability of PCOS is significant, with familial patterns suggesting that genetic predisposition may interact with environmental factors to trigger the condition. This genetic link underscores the importance of understanding family medical history when assessing risk for PCOS.
Lifestyle Link
Lifestyle factors have a profound impact on the severity of PCOS symptoms. Sedentary habits, poor dietary choices, and high-stress levels can exacerbate hormonal imbalances and insulin resistance.
- Sedentary Lifestyle: Lack of physical activity contributes to weight gain and worsens insulin resistance. Regular exercise is crucial for managing weight and improving insulin sensitivity.
- Diet: Diets high in processed foods, sugars, and unhealthy fats can lead to weight gain and increased insulin resistance. A balanced diet rich in whole foods, such as fruits, vegetables, whole grains, and lean proteins, is essential for managing PCOS symptoms.
- Stress: Chronic stress can disrupt hormonal balance and exacerbate insulin resistance. Stress management techniques, such as mindfulness, yoga, and regular physical activity, can help mitigate these effects.
The Long-Term Health Risks: More Than Just a Reproductive Disorder
Polycystic ovary syndrome (PCOS) is often misunderstood as a condition that solely affects fertility or appearance. However, the reality is much more alarming. If left untreated, PCOS can have severe long-term, life-altering health implications that extend far beyond reproductive concerns.
Type 2 Diabetes
Women with PCOS are at a significantly higher risk of developing type 2 diabetes, with studies suggesting they are up to four times more likely to be affected compared to women without PCOS. This increased risk is primarily driven by insulin resistance, a hallmark feature of PCOS. Insulin resistance leads to elevated blood sugar levels, which can progress to type 2 diabetes if left unchecked.
Cardiovascular Disease
The hormonal imbalances and metabolic challenges associated with PCOS can significantly increase the risk of cardiovascular disease. Women with PCOS have a higher prevalence of cardiovascular disease risk factors, such as:
- Dyslipidemia: PCOS is linked to an atherogenic lipid profile, characterized by elevated triglycerides, low HDL cholesterol, and small, dense LDL particles.
- Hypertension: Studies have shown that women with PCOS have a higher risk of developing high blood pressure compared to their peers without PCOS.
- Obesity: Excess weight, particularly abdominal obesity, is common in women with PCOS and can exacerbate other cardiovascular risk factors.
These factors contribute to the increased risk of heart disease, heart attacks, and strokes in women with PCOS.
Mental Health Struggles
The emotional burden of dealing with PCOS-related symptoms, such as excess hair growth, acne, and weight gain, combined with hormonal imbalances, can take a toll on mental health. Women with PCOS have a higher prevalence of anxiety, depression, and body image issues compared to women without the condition.
Endometrial Cancer
Irregular periods, a hallmark of PCOS, can lead to prolonged exposure to estrogen without ovulation. This imbalance can increase the risk of endometrial hyperplasia and endometrial cancer.
Sleep Apnea
The link between obesity, a common complication of PCOS, and sleep apnea adds another layer to the condition's seriousness. Sleep apnea is characterized by repeated episodes of breathing cessation during sleep, leading to poor sleep quality and increased cardiovascular risk.
PCOS and Fertility: Navigating the Emotional Rollercoaster
Polycystic ovary syndrome (PCOS) is a complex hormonal disorder that significantly impacts fertility, often leading to emotional distress for those affected. Understanding the challenges of conception associated with PCOS, as well as the available treatments, is crucial for women navigating this journey.
Challenges in Conception
PCOS is one of the leading causes of infertility, primarily due to its disruption of ovulation. Women with PCOS often experience irregular menstrual cycles or may not ovulate at all, a condition known as anovulation. This irregularity can make it difficult to predict fertile windows, complicating efforts to conceive.
The emotional toll of infertility can be profound. Women may experience feelings of frustration, inadequacy, and anxiety as they confront the challenges of trying to conceive. The societal pressures surrounding motherhood can exacerbate these feelings, making it essential to address both the physical and emotional aspects of fertility challenges in PCOS.
The Impact of Hormonal Imbalances
PCOS is characterized by hormonal imbalances, particularly elevated levels of androgens (male hormones) and insulin. These imbalances can lead to several fertility-related issues:
- Irregular Ovulation: The hormonal disruption can prevent the ovaries from releasing mature eggs regularly, making conception challenging.
- Uterine Lining Issues: Even if ovulation occurs, hormonal imbalances can affect the uterine lining, preventing it from developing properly for implantation of a fertilized egg.
- Increased Risk of Pregnancy Complications: Women with PCOS who do become pregnant face higher risks of complications such as gestational diabetes, preeclampsia, and miscarriage.
Fertility Treatments
Despite the challenges posed by PCOS, modern medical advancements offer hope for women seeking to conceive. Here are some common fertility treatments and strategies:
1. Lifestyle Modifications
Adopting a healthy lifestyle can significantly improve fertility outcomes for women with PCOS. Key strategies include:
- Weight Management: Even a modest weight loss of 5-10% can help restore normal ovulation and improve the chances of conception. A registered dietitian can provide personalized guidance on sustainable weight loss strategies.
- Balanced Diet: Focusing on a diet rich in whole grains, fruits, vegetables, lean proteins, and healthy fats can help manage insulin levels and support overall health.
- Regular Exercise: Engaging in regular physical activity, such as brisk walking or swimming, can help manage weight, reduce insulin resistance, and regulate hormone levels.
- Stress Management: Techniques such as yoga, meditation, and mindfulness can help alleviate stress, which may further improve fertility.
2. Medical Treatments
If lifestyle changes alone are insufficient, medical interventions may be necessary. Common fertility treatments for women with PCOS include:
- Ovulation-Inducing Medications: Medications such as clomiphene citrate (Clomid) or letrozole (Femara) are often prescribed to stimulate ovulation. These medications can help women with PCOS to ovulate regularly, increasing the chances of conception.
- Metformin: This medication, commonly used to treat insulin resistance, can also help improve ovulation in women with PCOS.
- Injectable Gonadotropins: For women who do not respond to oral medications, injectable hormones may be used to stimulate the ovaries.
- Assisted Reproductive Technologies (ART): In cases where other treatments are ineffective, options such as intrauterine insemination (IUI) or in vitro fertilization (IVF) may be considered. IVF has been shown to have higher success rates for women with PCOS compared to other methods.
The Importance of Early Diagnosis
Early diagnosis of PCOS is crucial for effective management and treatment. Women experiencing symptoms such as irregular periods, excessive hair growth, or weight gain should consult a healthcare provider for evaluation. A proper diagnosis can lead to timely interventions that improve fertility outcomes and overall health.
Emotional Support and Counseling
Navigating the emotional rollercoaster of infertility can be overwhelming. Seeking support from mental health professionals, support groups, or counseling can provide valuable coping strategies and emotional relief. Connecting with others who share similar experiences can also help reduce feelings of isolation and anxiety.
Managing PCOS with Lifestyle and Medical Interventions
Polycystic ovary syndrome (PCOS) is a multifaceted condition that affects women’s reproductive and overall health. A holistic approach to managing PCOS combines lifestyle changes with medical interventions, addressing both the physical and emotional aspects of the disorder. This comprehensive strategy can empower women to take control of their health and improve their quality of life.
Lifestyle Changes
For many women, lifestyle adjustments are the cornerstone of managing PCOS. Key areas of focus include diet, exercise, and stress management.
Diet
A balanced diet plays a crucial role in managing PCOS symptoms. Research suggests that a diet rich in whole foods and low in refined sugars can improve insulin sensitivity and support hormonal balance.
- Whole Foods: Emphasizing whole grains, fruits, vegetables, lean proteins, and healthy fats can help regulate blood sugar levels and reduce inflammation.
- Reduced Refined Sugars: Limiting processed foods and sugars can help manage weight and improve metabolic health, which is vital for women with PCOS.
- Nutrient Supplementation: Certain vitamins and minerals have been shown to be beneficial for women with PCOS. These include:
- Inositol: Emerging research suggests that inositol supplements can improve insulin sensitivity and ovarian function.
- Vitamin D: Many women with PCOS have low levels of vitamin D, and supplementation may help improve reproductive function.
- Omega-3 Fatty Acids: These can help reduce inflammation and improve metabolic profiles.
Exercise
Regular physical activity is essential for managing PCOS. Exercise can improve insulin sensitivity, aid in weight management, and help regulate menstrual cycles.
- Types of Exercise: A combination of aerobic exercises (like walking, jogging, or swimming) and strength training can be particularly effective. High-intensity interval training (HIIT) has also shown promise in improving insulin sensitivity and cardiovascular health.
- Consistency: Aim for at least 150 minutes of moderate-intensity exercise per week. Finding activities that are enjoyable can help maintain motivation and adherence.
Stress Management
Chronic stress can exacerbate PCOS symptoms by disrupting hormonal balance. Implementing stress management techniques is crucial for overall well-being.
- Mindfulness and Meditation: Practices such as mindfulness meditation, yoga, and deep-breathing exercises can help reduce stress and improve emotional health.
- Counseling and Support Groups: Seeking professional help or joining support groups can provide emotional support and coping strategies for dealing with the challenges of PCOS.
Medical Treatments
While lifestyle changes are fundamental, medical interventions may also be necessary to manage PCOS effectively.
Hormonal Birth Control
Hormonal contraceptives are often prescribed to help regulate menstrual cycles and reduce symptoms associated with elevated androgen levels, such as acne and hirsutism. These medications can help restore hormonal balance and provide relief from some of the physical symptoms of PCOS.
Anti-Androgens
Medications such as spironolactone can be prescribed to reduce excess hair growth and acne by blocking the effects of androgens. This treatment can be particularly beneficial for women who experience significant hirsutism.
Metformin
Metformin is an insulin-sensitizing medication commonly used to manage insulin resistance in women with PCOS. It can help improve menstrual regularity and promote ovulation, making it a valuable option for those trying to conceive.
Emerging Therapies
Recent research has explored the potential benefits of various supplements and alternative therapies for managing PCOS symptoms:
- Inositol Supplements: These have gained popularity for their role in improving insulin sensitivity and ovarian function.
- Herbal Remedies: Some women may benefit from herbal supplements, such as spearmint tea for reducing hirsutism or cinnamon for improving insulin sensitivity. However, it is essential to consult with a healthcare provider before starting any herbal treatments.
The Role of Mental Health Care
Given the mental health challenges associated with PCOS, a holistic treatment plan should include counseling or therapy to address anxiety, depression, and self-esteem issues. Women with PCOS often experience feelings of frustration and isolation due to their symptoms, making mental health support a critical component of comprehensive care.
- Therapeutic Approaches: Cognitive-behavioral therapy (CBT) and mindfulness-based therapies can be effective in addressing the emotional aspects of living with PCOS.
- Support Networks: Connecting with others who share similar experiences can provide valuable emotional support and reduce feelings of isolation.
Promising Treatments on the Horizon for PCOS
Recent studies have shed light on innovative treatment options for polycystic ovary syndrome (PCOS), a condition that affects a significant number of women worldwide. This research highlights the potential of inositol supplements, anti-inflammatory diets, and advancements in genetic research to provide more personalized and effective management strategies for PCOS.
- Inositol Supplements: One of the most promising developments in PCOS treatment is the use of myo-inositol supplements. Research indicates that inositol can significantly improve insulin sensitivity and restore hormonal balance in women with PCOS.
- Mechanism of Action: Inositol plays a crucial role in cellular signaling and is involved in the insulin signaling pathway. By enhancing insulin sensitivity, inositol can help lower elevated insulin levels, which is a common issue in women with PCOS. This, in turn, can lead to improved ovarian function and regular menstrual cycles.
- Clinical Evidence: A study published in the Journal of Endocrinological Investigation found that women who supplemented with myo-inositol experienced improvements in metabolic parameters, including reduced insulin resistance and improved ovarian function, leading to better fertility outcomes.
Emerging Therapies: Anti-Inflammatory Diets
Research is increasingly focusing on the role of diet in managing PCOS, particularly the benefits of anti-inflammatory dietary approaches.
- Anti-Inflammatory Diets: Studies have shown that adopting an anti-inflammatory diet can lead to significant improvements in metabolic, endocrine, and reproductive profiles in women with PCOS. A Mediterranean-inspired diet, which is rich in fruits, vegetables, whole grains, healthy fats, and lean proteins, has been associated with reduced inflammation and improved insulin sensitivity.
- Clinical Findings: A clinical trial involving overweight and obese women with PCOS demonstrated that participants following an anti-inflammatory diet for 12 weeks experienced moderate weight loss and significant improvements in hormonal balance, menstrual regularity, and metabolic health markers, such as glucose levels and lipid profiles. The study reported a 63% restoration of menstrual cyclicity and a 12% spontaneous pregnancy rate among participants.
Genetic Research: Personalized Treatments
Advancements in genetic research are paving the way for more personalized treatment options for PCOS.
- Genetic Studies: Researchers are investigating the genetic underpinnings of PCOS to identify specific genetic markers that may predict an individual's response to various treatments. This research aims to tailor interventions based on a woman’s unique genetic makeup, potentially improving treatment efficacy.
- Future Implications: Personalized medicine could revolutionize the management of PCOS by allowing healthcare providers to offer targeted therapies that address the specific hormonal and metabolic imbalances present in each patient. This approach could lead to more effective management strategies and better overall outcomes for women with PCOS.
Mental Health and PCOS: The Silent Struggle
Polycystic ovary syndrome (PCOS) is a complex hormonal disorder that affects many aspects of a woman's health, including mental well-being. The emotional impact of PCOS is profound, often leading to significant mental health challenges that can be overlooked in discussions about the condition. Understanding these challenges and the stigma surrounding them is crucial for empowering women to seek the help they need.
Emotional Impact
Dealing with PCOS often brings a unique set of mental health challenges. Women with PCOS frequently experience:
- Body Image Issues: Symptoms such as weight gain, hirsutism (excess hair growth), and acne can lead to dissatisfaction with body image. These physical changes can significantly impact self-esteem and contribute to feelings of inadequacy.
- Fertility Struggles: Infertility is a common issue for women with PCOS, as the condition disrupts normal ovulation. The emotional toll of trying to conceive can be overwhelming, leading to anxiety, depression, and feelings of isolation. Research indicates that approximately 40% of women with PCOS experience depression during their reproductive years, often exacerbated by fertility challenges.
- Anxiety and Depression: Women with PCOS are about three times more likely to experience anxiety and depression compared to those without the condition. The interplay of hormonal imbalances, physical symptoms, and societal pressures can create a perfect storm for mental health struggles.
Breaking the Stigma
Many women suffer in silence, believing their symptoms are a personal failure rather than part of a diagnosable condition. This stigma can prevent them from seeking help and support. Increased public awareness and open dialogue about PCOS can empower women to recognize their experiences as valid and deserving of attention.
- Need for Awareness: Many women are unaware that their struggles with body image, fertility, and mental health are linked to PCOS. Raising awareness about the condition and its psychological effects can encourage women to seek appropriate medical and psychological support.
- Encouraging Open Dialogue: Creating safe spaces for women to discuss their experiences with PCOS can help reduce feelings of isolation. Support groups and online forums can provide valuable resources and connections for those navigating the challenges of the condition.
Research Insights
Recent studies have highlighted the significant mental health concerns associated with PCOS. For instance, a study published in the Journal of Behavioral Health Services & Research found that menstrual irregularities were the strongest predictor of mental health issues among women with PCOS. This underscores the need for healthcare providers to address mental health as part of a comprehensive treatment plan for PCOS.
Another study indicated that women with PCOS often report higher levels of psychological distress compared to the general population, with symptoms such as anxiety, depression, and body dissatisfaction being prevalent. These findings emphasize the importance of screening for mental health issues in women diagnosed with PCOS.
The Role of Mental Health Care
Given the mental health challenges associated with PCOS, holistic treatment should include counseling or therapy to address anxiety, depression, and self-esteem issues.
- Therapeutic Approaches: Cognitive-behavioral therapy (CBT) and mindfulness-based therapies can be effective in addressing the emotional aspects of living with PCOS. These interventions can help women develop coping strategies and improve their overall mental health.
- Support Networks: Connecting with others who share similar experiences can provide valuable emotional support. Support groups, whether in-person or online, can help women feel less isolated and more understood.
Conclusion
Empowering women with PCOS involves not only providing them with the necessary medical resources but also fostering a supportive community where they can share their experiences and challenges. Support groups and online forums can offer invaluable emotional support and practical advice, helping women feel less isolated in their struggles.
By raising awareness, promoting comprehensive treatment options, and encouraging open dialogue about PCOS, we can help women not only manage their condition but thrive in spite of it. The journey toward better health and well-being for women with PCOS is ongoing, and collective efforts from healthcare providers, researchers, and the community are essential in making a meaningful impact.
In conclusion, while PCOS presents unique challenges, it is a condition that can be managed effectively. With the right knowledge, support, and proactive steps, women with PCOS can take control of their health and lead fulfilling lives. By sharing knowledge and fostering a sense of empowerment, we can help women with PCOS overcome the challenges posed by this complex condition and improve their overall quality of life.